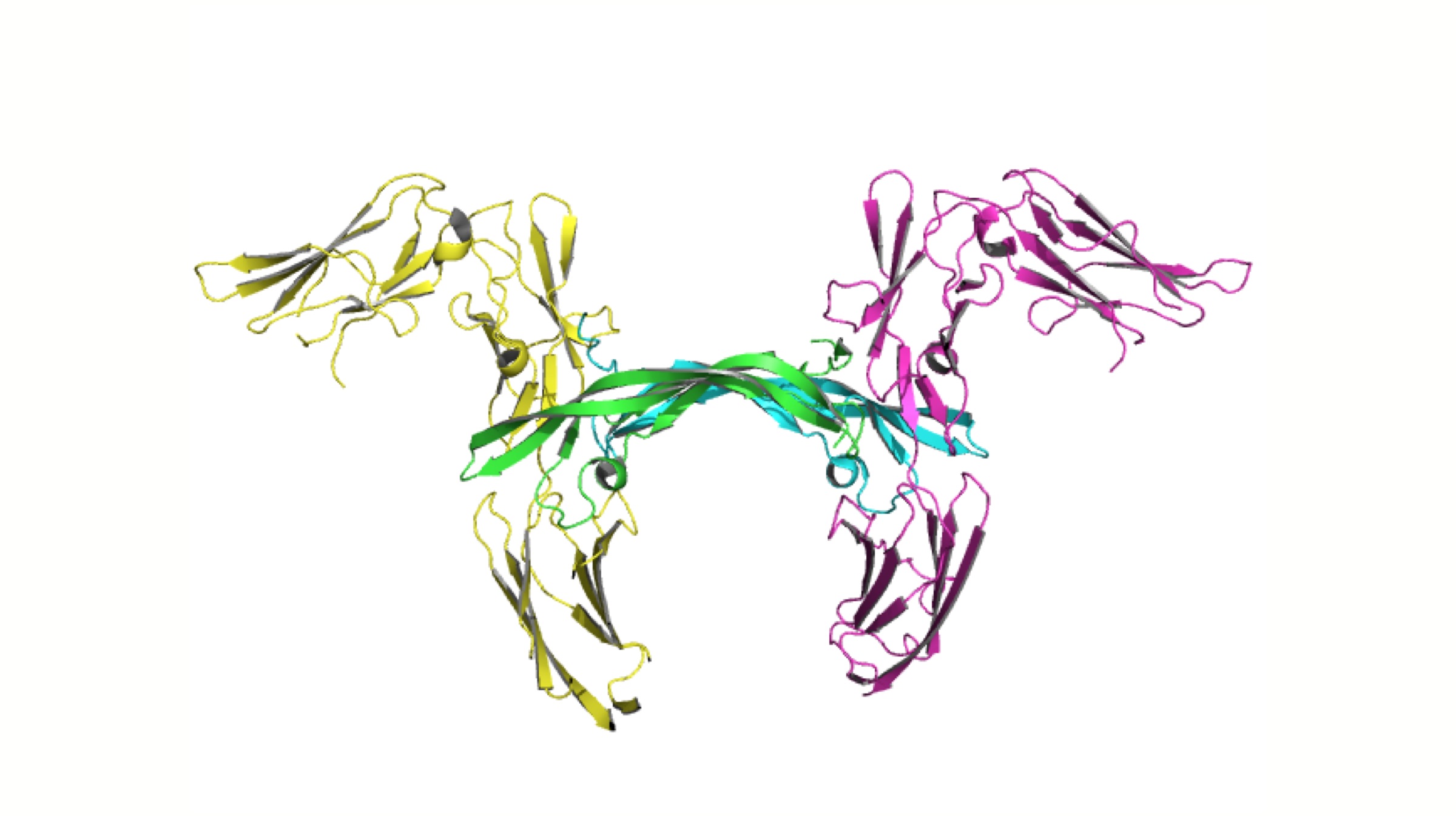
A huge number of people perish each year across the globe due to a shortage of blood transfusion stocks. On paper, almost 55 million litres of blood is donated annually worldwide, but in reality, incompatibility between the blood types implies that a person may not always receive a transfusion. However, researchers at the University of British Columbia have discovered a method using which type A blood can be converted into type O universal blood type.
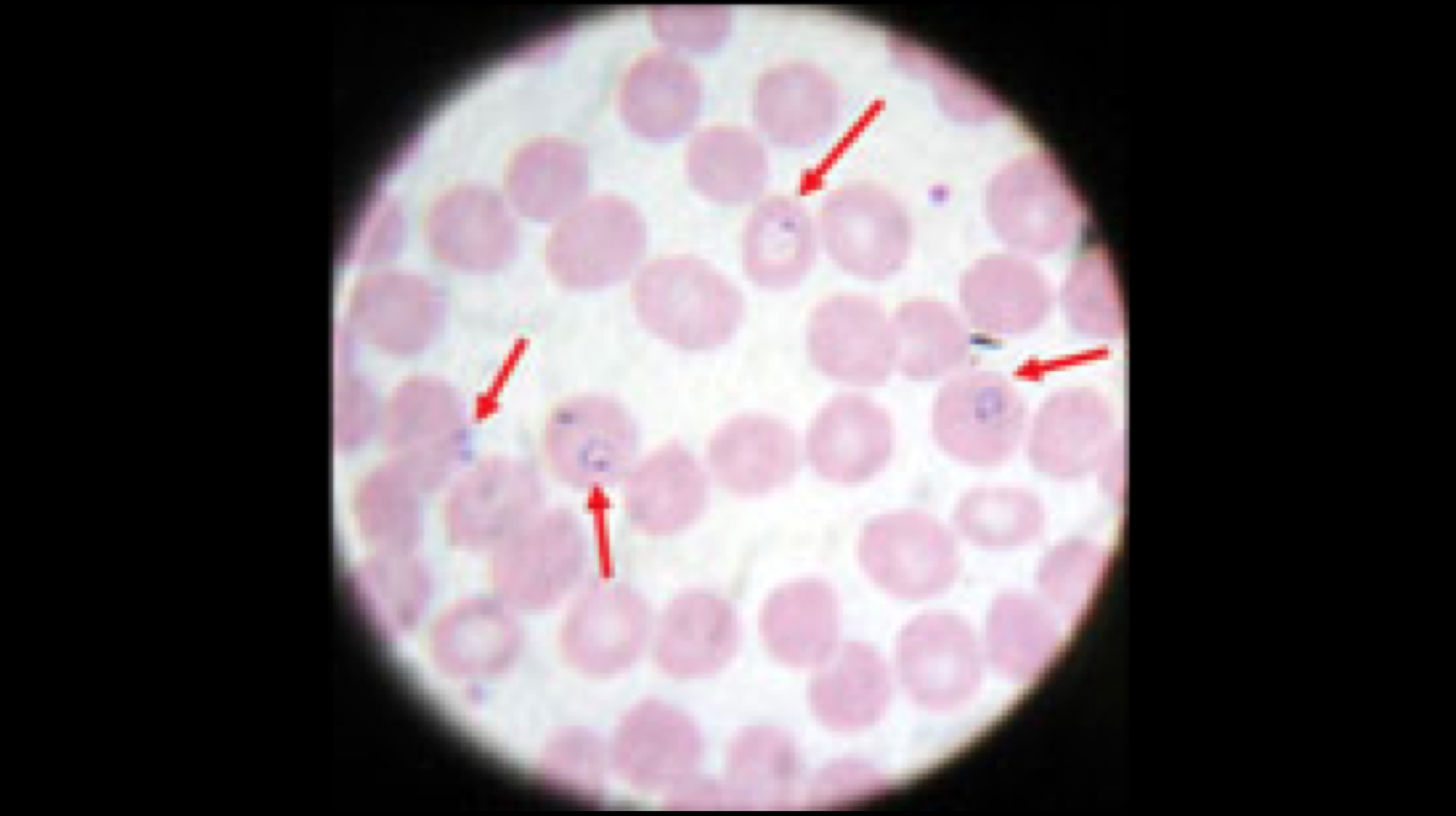
Type O blood is compatible with anyone who has Rhesus (Rh) positive blood. Hence, it is considered as the universal blood type, since it can be transfused with anyone who has A+, B+, AB+, or O+ blood, which comprises about 75% of the total population. Postdoctoral researcher Peter Rahfeld has discovered a way via which enzymes can be used to transform type A red blood cells into universal type O blood cells. As per reports, this development can potentially double the stock of transfusion blood in the world.
If a person with type A blood is accidentally transfused with type B blood, the B antigens present in the transfused blood would cause the anti-B antibodies to attack the blood cells in a fatal manner, which would consequently result in the death of the person. On the other hand, type O red blood cells don’t have both the A and B antigens on their surface, instead, they harbour a neutral “H” antigen instead. This means anyone can be compatible with the aforementioned blood type.
Also Read: Samsung’s 64 MP Sensor To Debut In A Redmi Smartphone
In order to convert blood types, the lead researcher and his team have made use of a bacterial enzyme that resides in the human gut to remove all traces of A antigens simply by converting them into H antigens. They further identified genes that encode two enzymes which can remove facilitating components of the A antigen. When the enzymes were added to type A blood, they stripped the blood of all A type antigens, essentially converting them to Universal Type O cells. These findings may significantly increase the number of lives saved across the globe. However, it will take a fair share of time for this research to be applied to humans on a large scale.

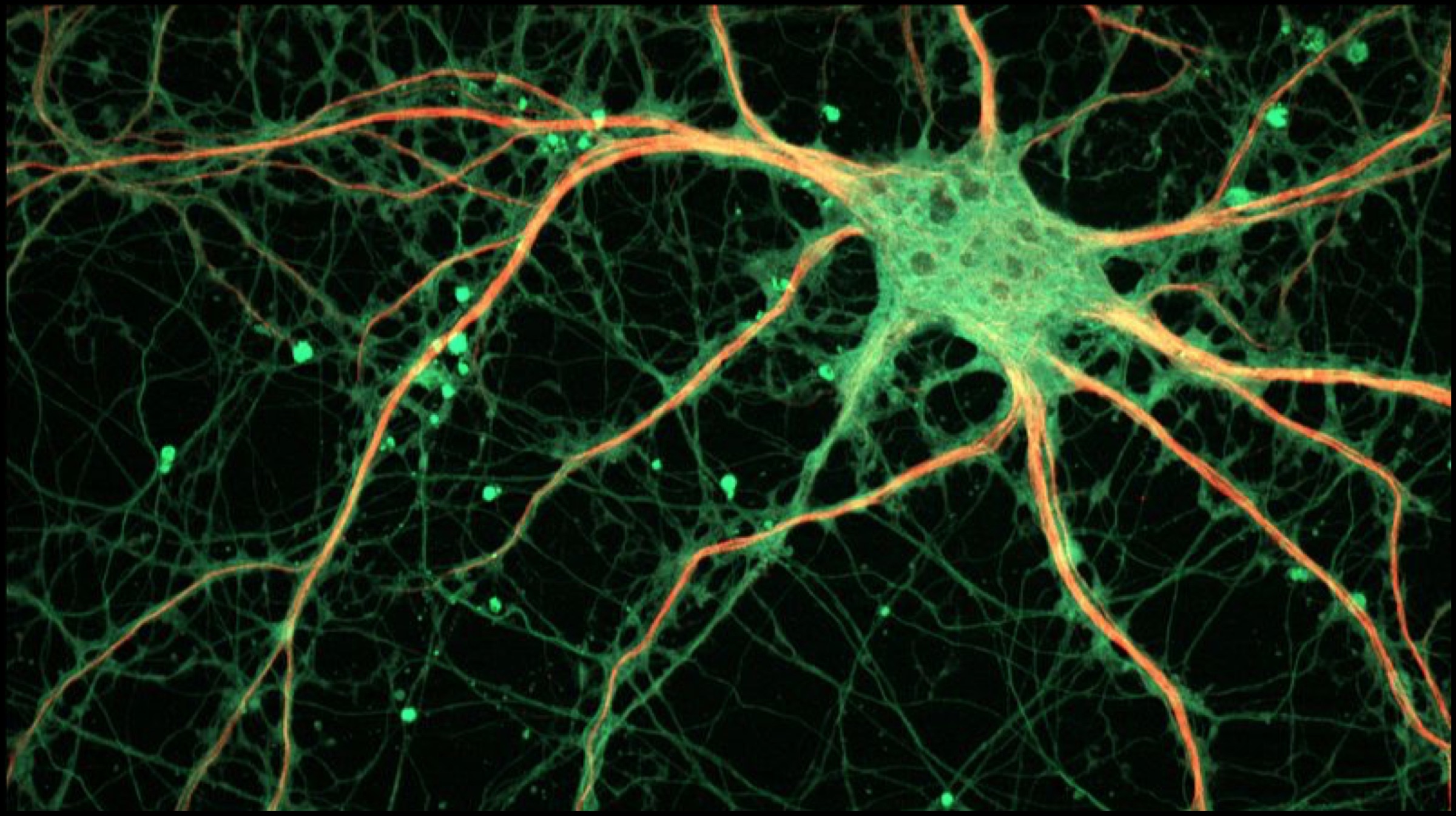
 Neural Stem Cells manufacture neurons, which are responsible for
Neural Stem Cells manufacture neurons, which are responsible for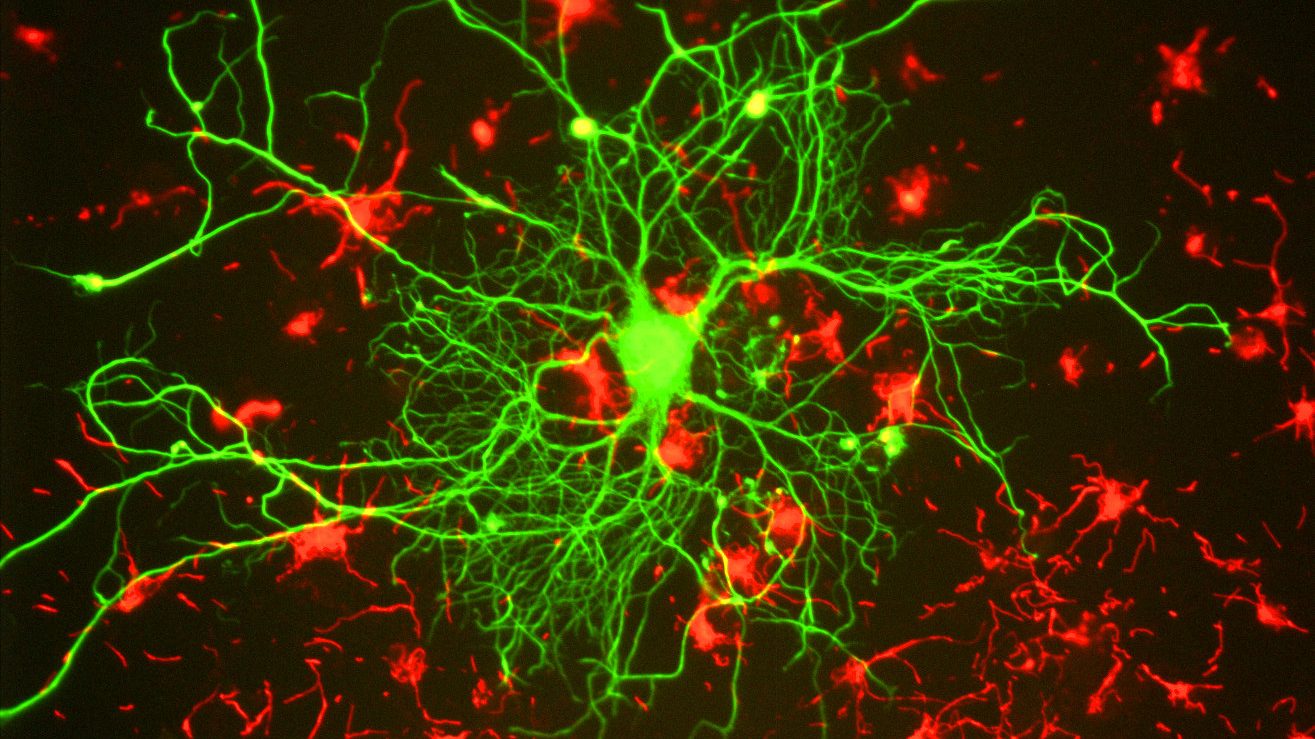


 Scientists from the University of Sussex worked in a collaboration with researchers from the University of Washington School of Medicine in Seattle, USA. The treatment involves the usage of ‘Receptor tyrosine kinase inhibitors’; which is a class of drug currently being used to treat cancer. A number of complex DNA sequencing techniques were implemented, and a new genetic basis of a brain aneurysm form was identified. Manuel Ferreira states that the mutations in the aforementioned gene were completely different from the ones that were previously detected in brain aneurysms.
Scientists from the University of Sussex worked in a collaboration with researchers from the University of Washington School of Medicine in Seattle, USA. The treatment involves the usage of ‘Receptor tyrosine kinase inhibitors’; which is a class of drug currently being used to treat cancer. A number of complex DNA sequencing techniques were implemented, and a new genetic basis of a brain aneurysm form was identified. Manuel Ferreira states that the mutations in the aforementioned gene were completely different from the ones that were previously detected in brain aneurysms.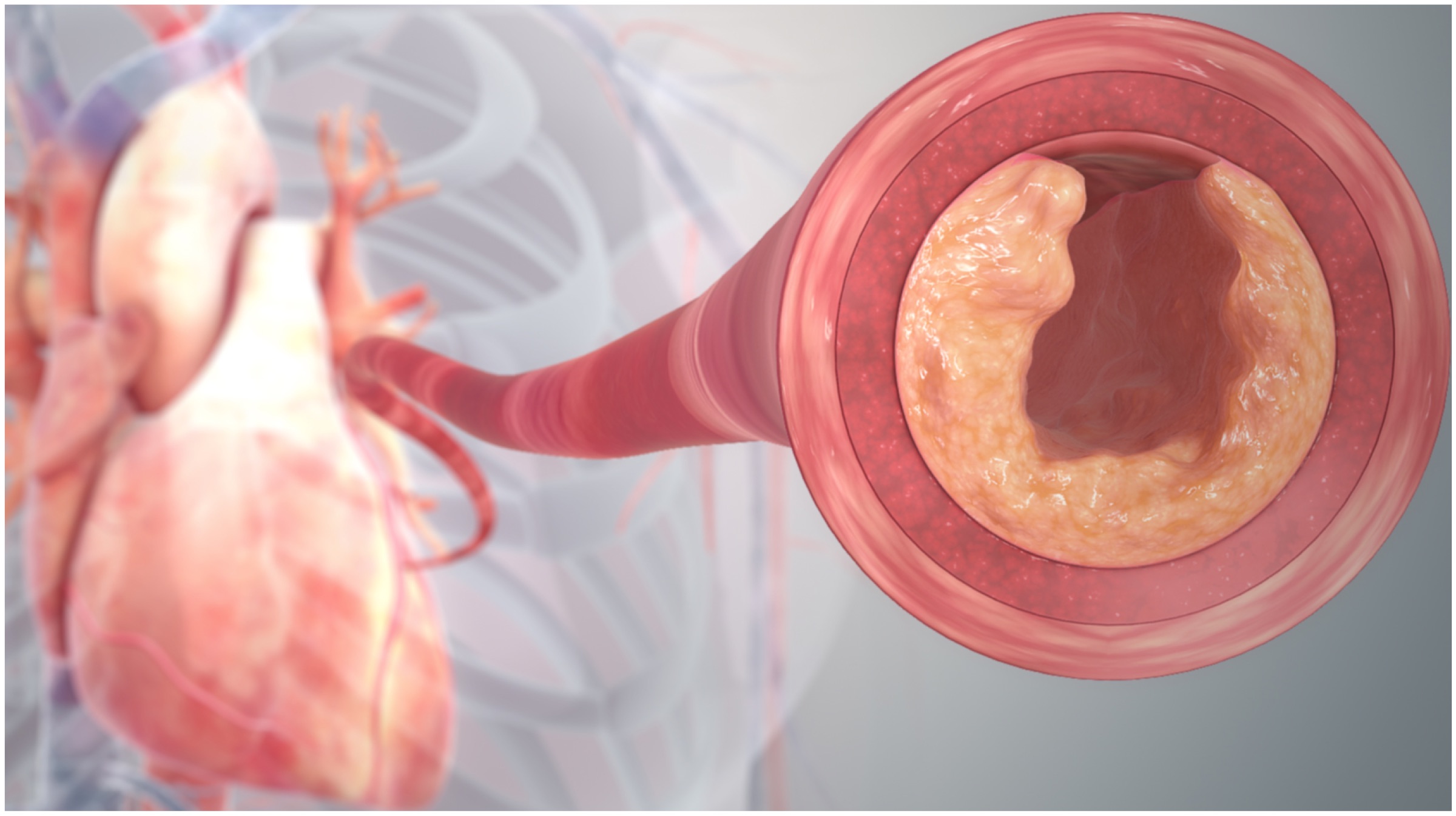 Also Read:
Also Read: 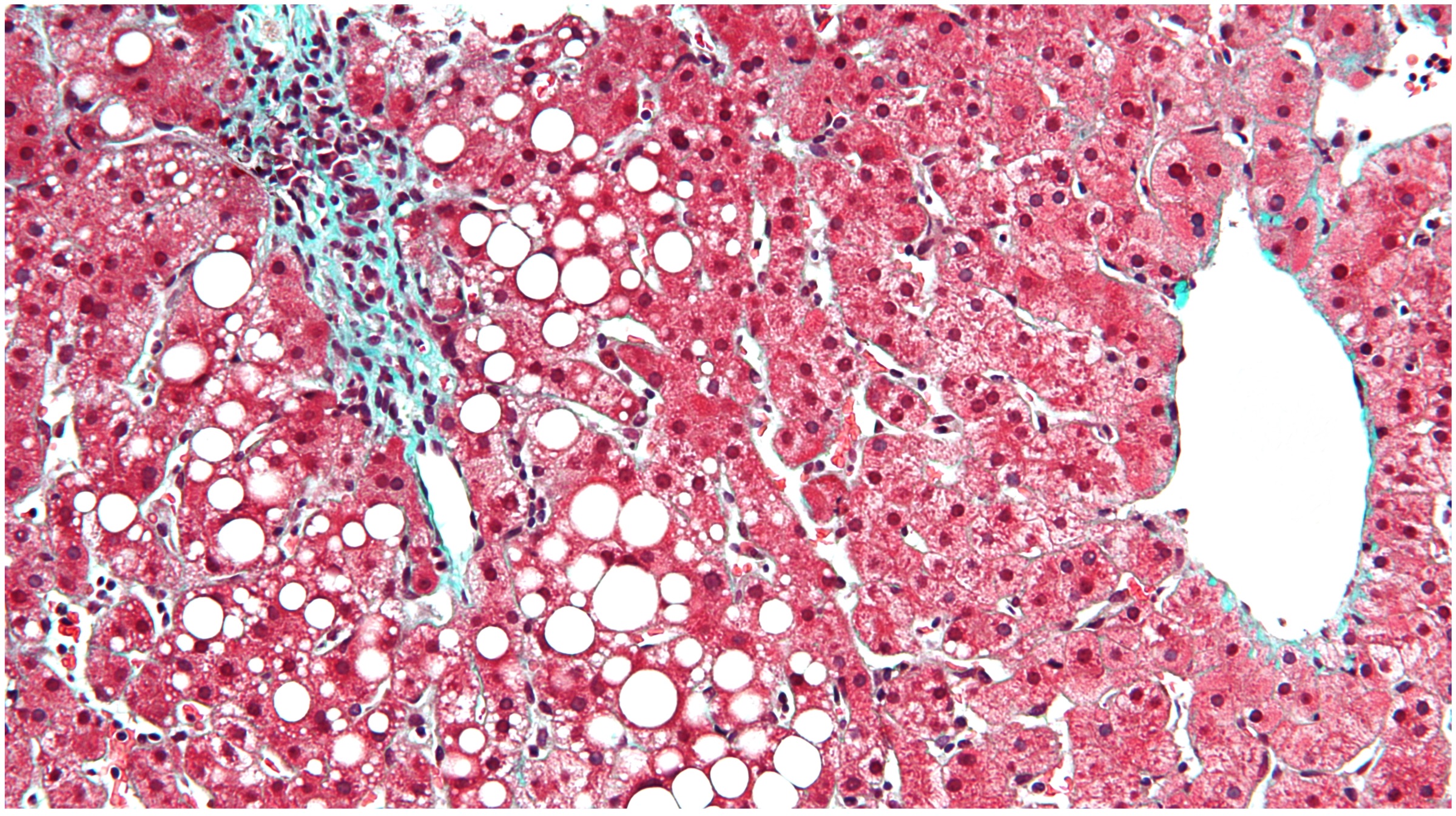

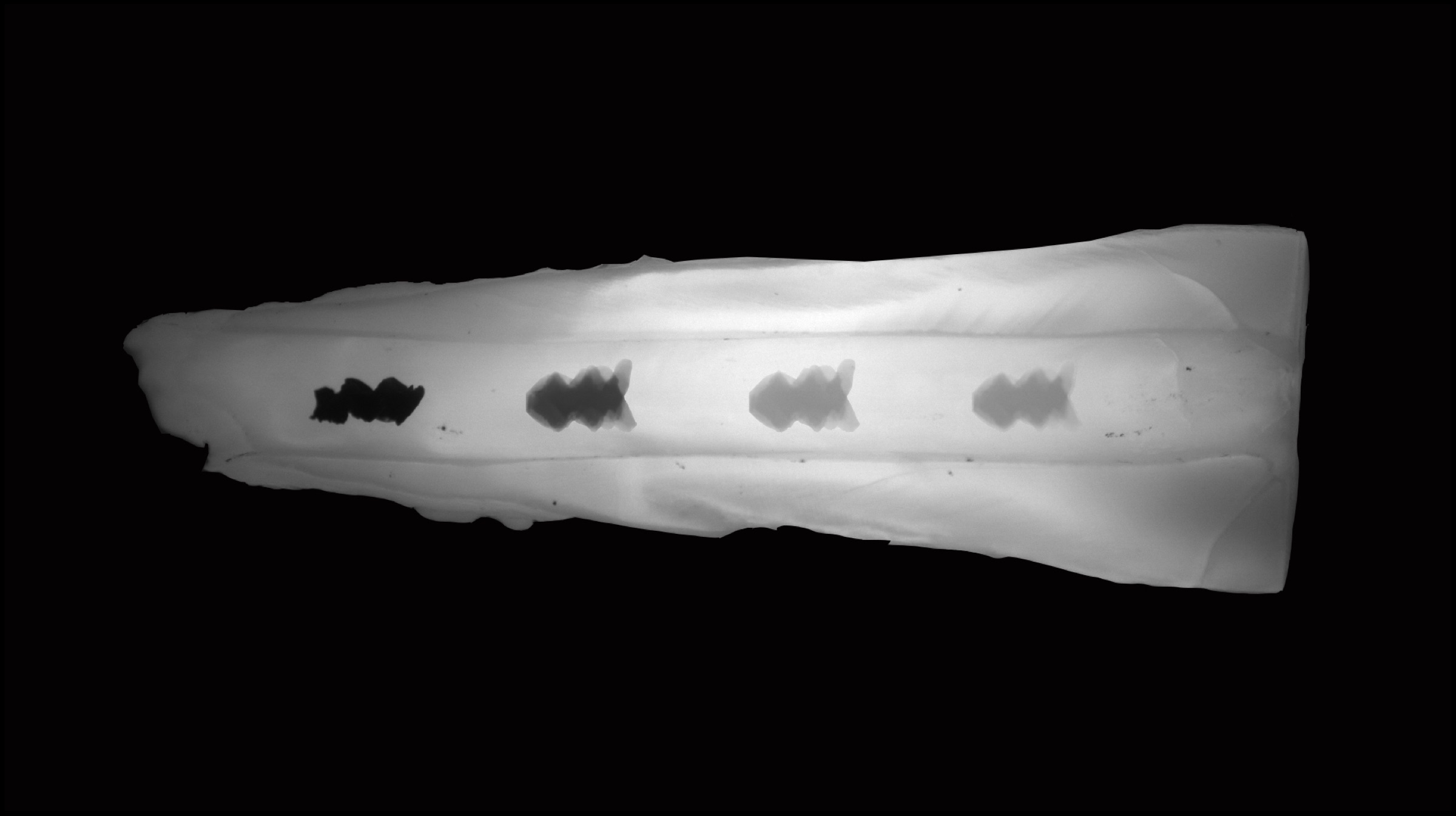
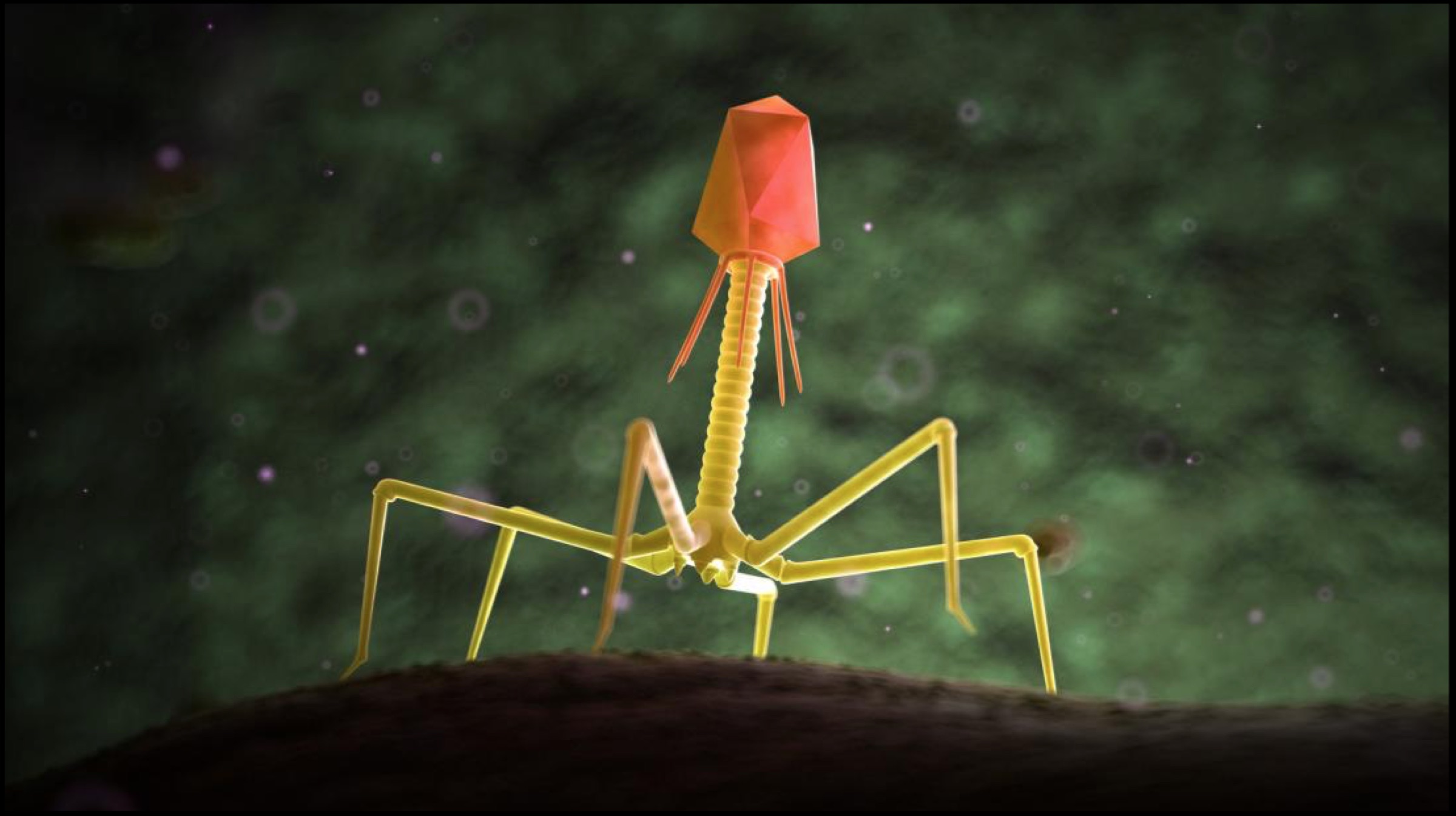 Researchers at the University of Pittsburgh in Pennsylvania and Howard Hughes Medical Institute (HHMI) in Chevy Chase have put forward evidence that suggests that a category of viruses known as “bacteriophages” can be the solution to antibiotic-resistant bacteria. These bacteria-eating viruses target and kill a variety of strains of bacteria that cause infection. An interesting fact to note is that there are an estimated 1031 bacteriophages on this planet, and different phages target different bacterial strains.
Researchers at the University of Pittsburgh in Pennsylvania and Howard Hughes Medical Institute (HHMI) in Chevy Chase have put forward evidence that suggests that a category of viruses known as “bacteriophages” can be the solution to antibiotic-resistant bacteria. These bacteria-eating viruses target and kill a variety of strains of bacteria that cause infection. An interesting fact to note is that there are an estimated 1031 bacteriophages on this planet, and different phages target different bacterial strains.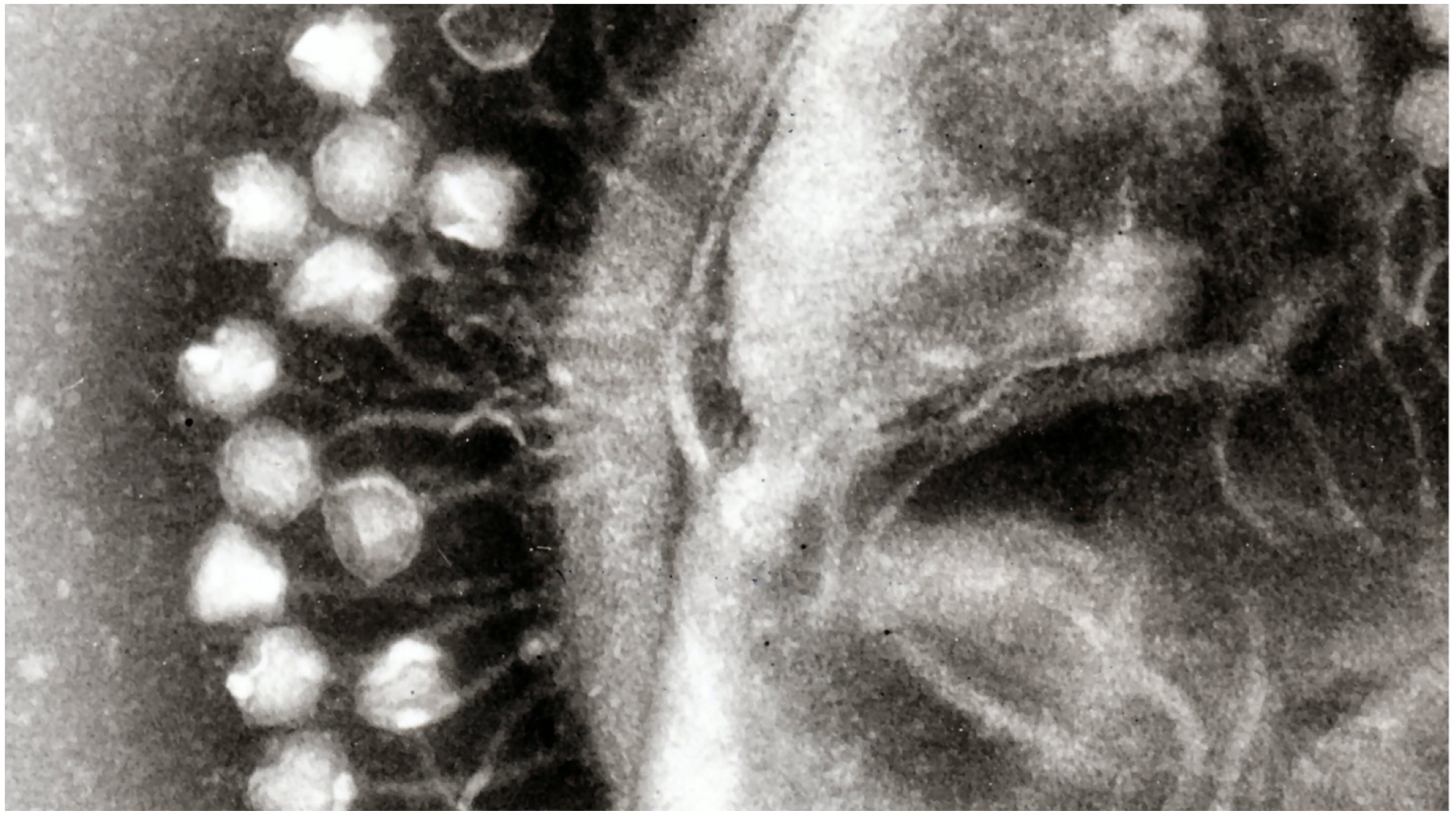 Using bacteriophages (or simply phages) to ward off infections is not a new idea at all. In fact, researchers from Britain, France and Russia were involved in similar investigations since the beginning of the 20th Century, which are proving to be fruitful just now owing to the advancements in research techniques. The “bacteria-attacking” technique was implemented in 2017, where a team of scientists lead by Professor Hatfull achieved a feat nothing short of a miracle.
Using bacteriophages (or simply phages) to ward off infections is not a new idea at all. In fact, researchers from Britain, France and Russia were involved in similar investigations since the beginning of the 20th Century, which are proving to be fruitful just now owing to the advancements in research techniques. The “bacteria-attacking” technique was implemented in 2017, where a team of scientists lead by Professor Hatfull achieved a feat nothing short of a miracle.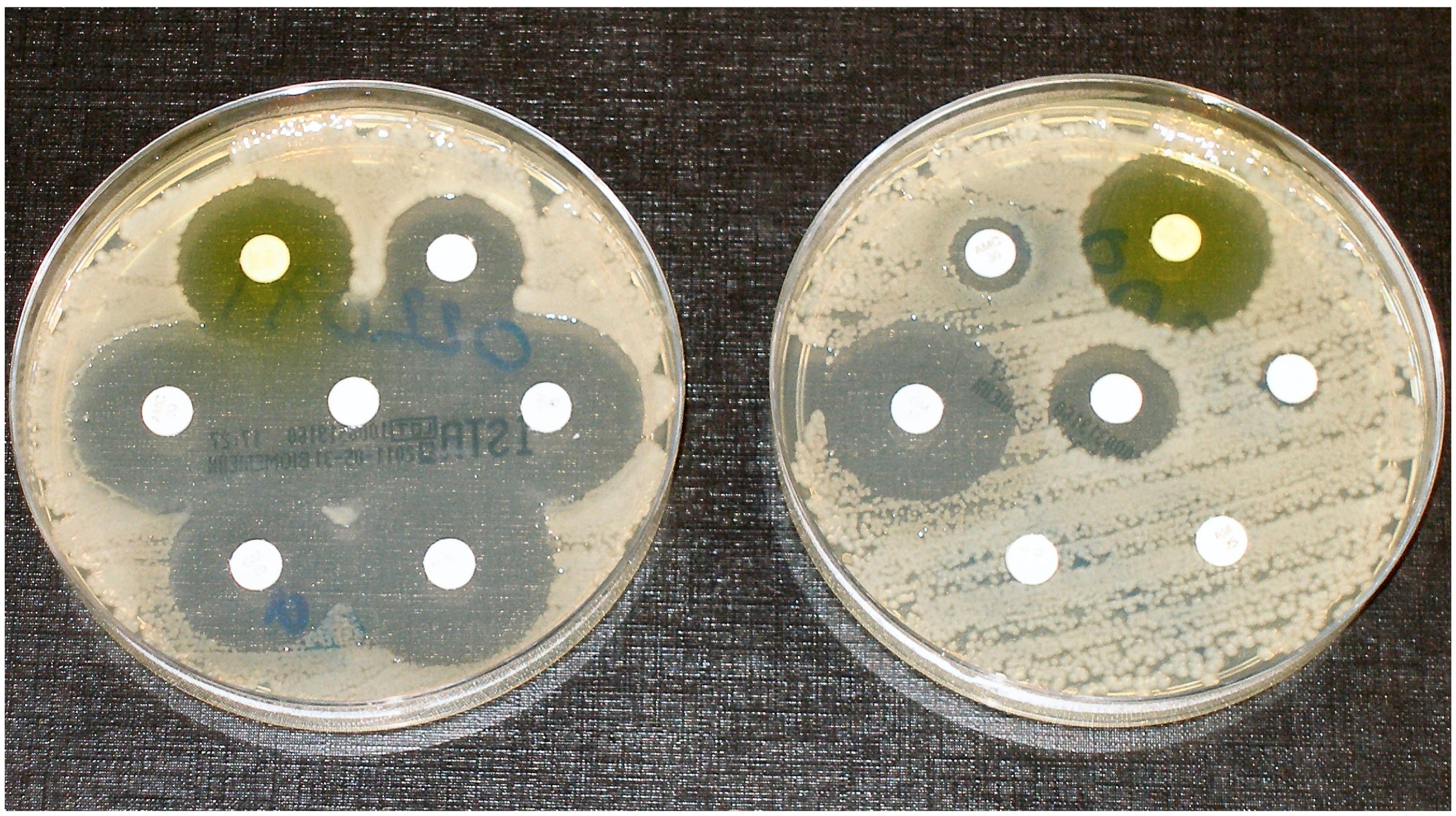 The team of scientists were able to treat an infection experienced by a 15-year-old patient with the help of carefully chosen phages. The patient suffered from cystic fibrosis, which increased the risk of infections because of a buildup of thick mucus in the lungs (and other organs). Moreover, the genetic condition is virtually incurable. After a double lung transplant, it was detected that the patient’s surgery wound was reddened because of a liver infection. Another patient with a similar condition also developed an infection after his surgery. When the infections showed signs of resistance to antibiotics, the scientists decided to use bacteriophages to kill the concerned bacteria.
The team of scientists were able to treat an infection experienced by a 15-year-old patient with the help of carefully chosen phages. The patient suffered from cystic fibrosis, which increased the risk of infections because of a buildup of thick mucus in the lungs (and other organs). Moreover, the genetic condition is virtually incurable. After a double lung transplant, it was detected that the patient’s surgery wound was reddened because of a liver infection. Another patient with a similar condition also developed an infection after his surgery. When the infections showed signs of resistance to antibiotics, the scientists decided to use bacteriophages to kill the concerned bacteria.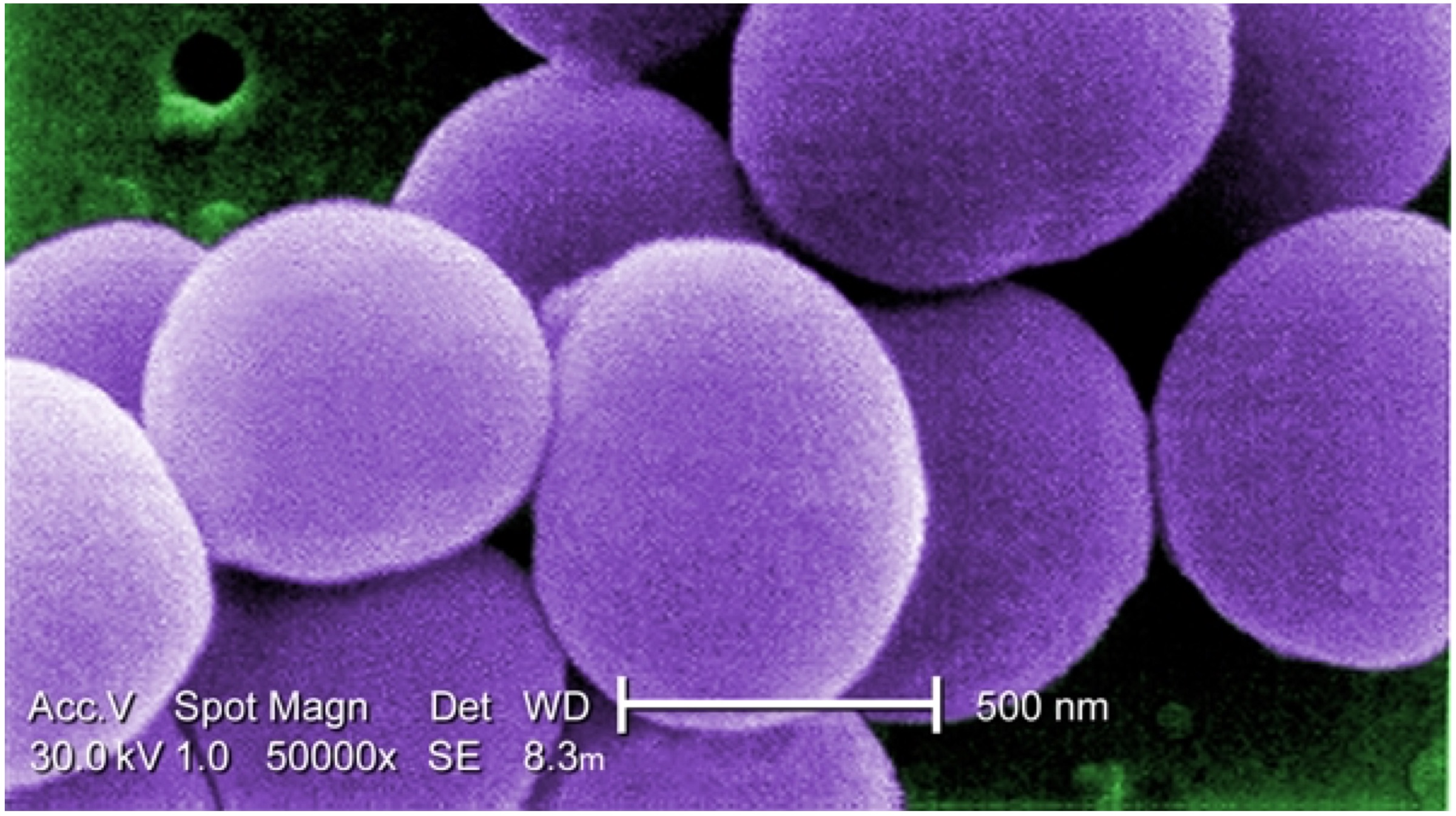 Also Read:
Also Read: 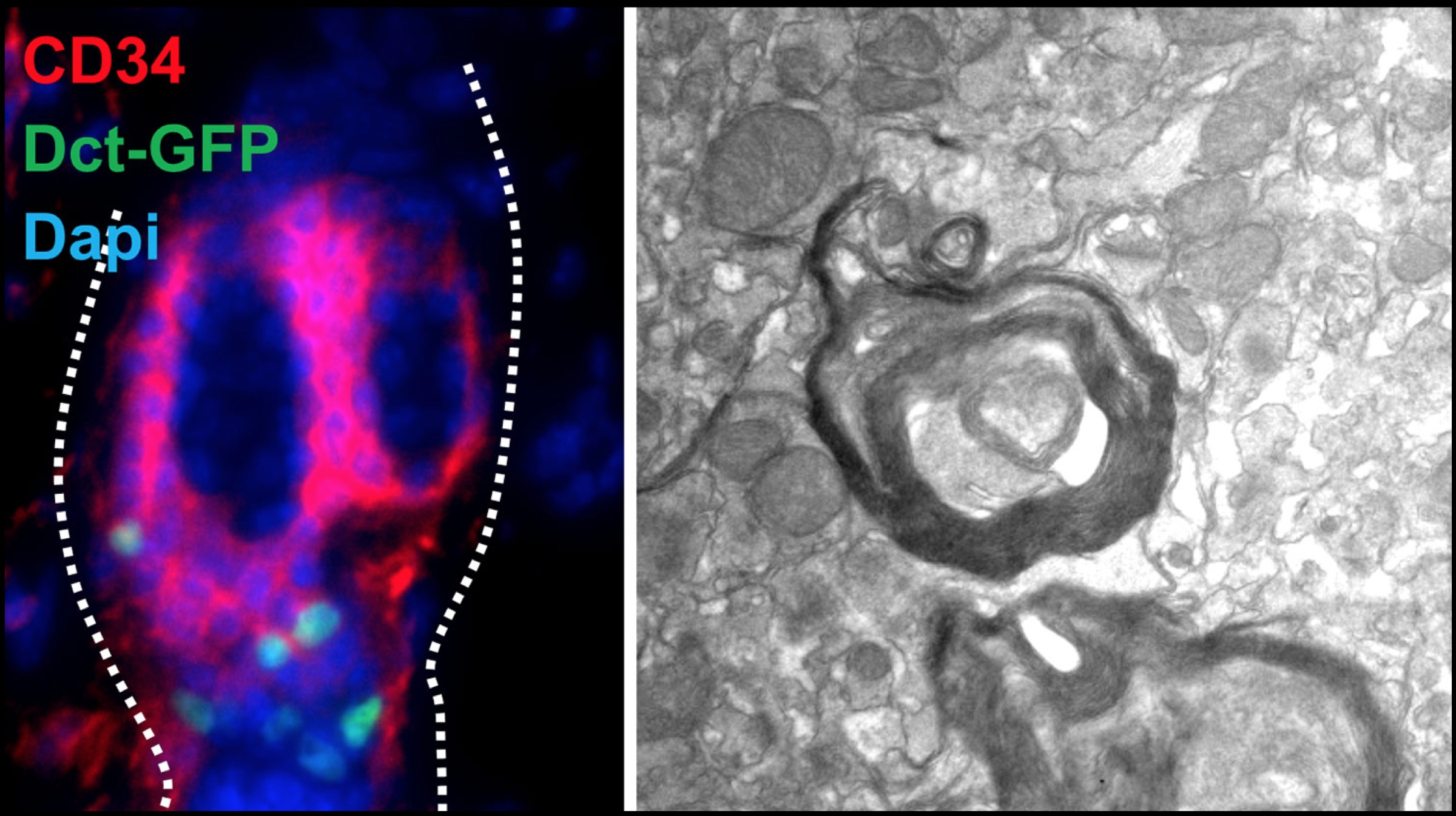
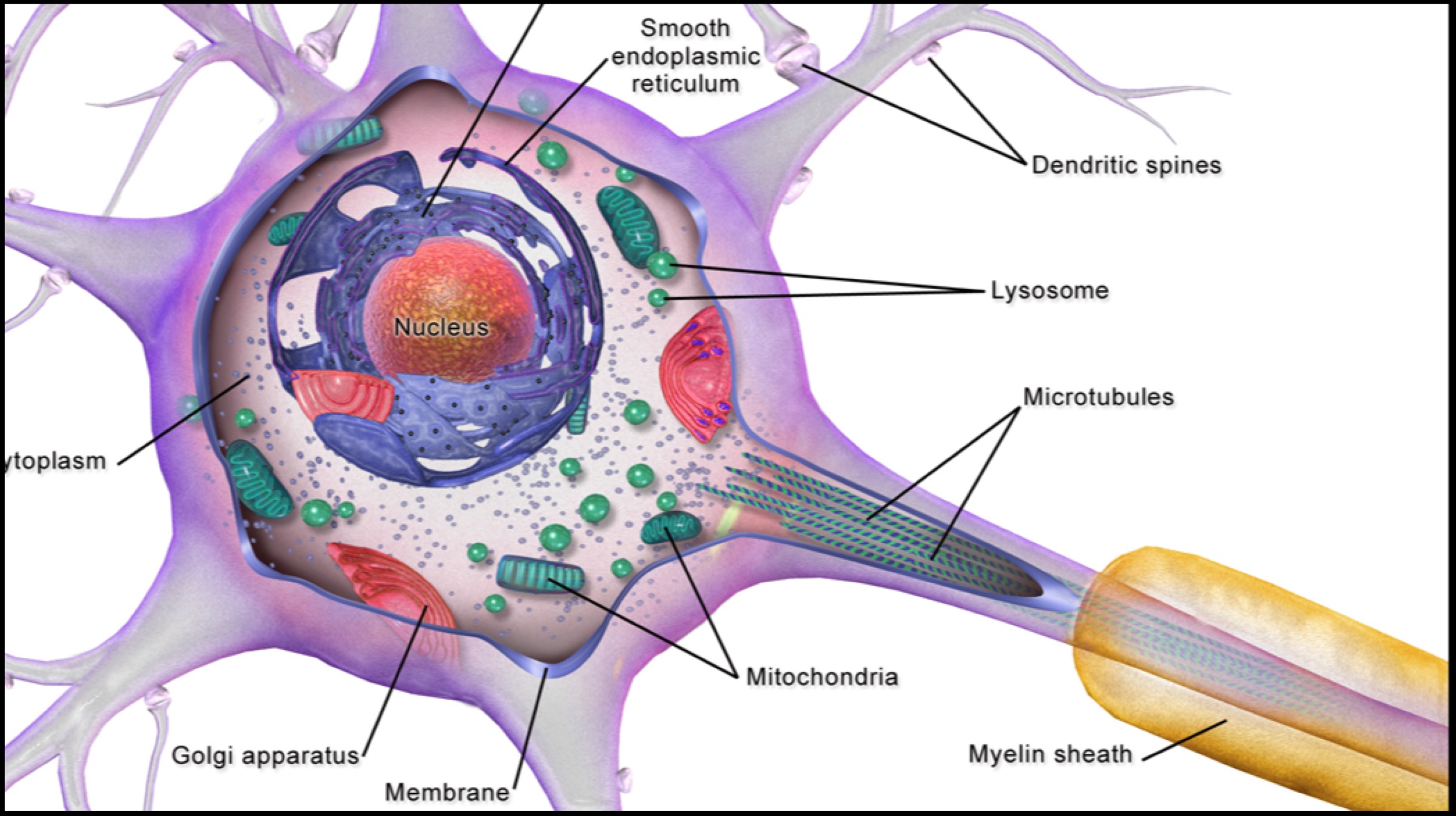 Research performed on mice yielded positive results. Restoration of myelin sheaths in mice led them to believe that stem cells could be a much simpler alternative to using embryonic stem cells. Since the human skin stem cells can be isolated, expanded and used therapeutically, they can possibly improve the chances of functional recovery in case of any injury to the neurons in the nervous system. Dr Thomas J. Hornyak, the lead investigator in the research plans to expand research into the aforementioned area using collected data.
Research performed on mice yielded positive results. Restoration of myelin sheaths in mice led them to believe that stem cells could be a much simpler alternative to using embryonic stem cells. Since the human skin stem cells can be isolated, expanded and used therapeutically, they can possibly improve the chances of functional recovery in case of any injury to the neurons in the nervous system. Dr Thomas J. Hornyak, the lead investigator in the research plans to expand research into the aforementioned area using collected data. 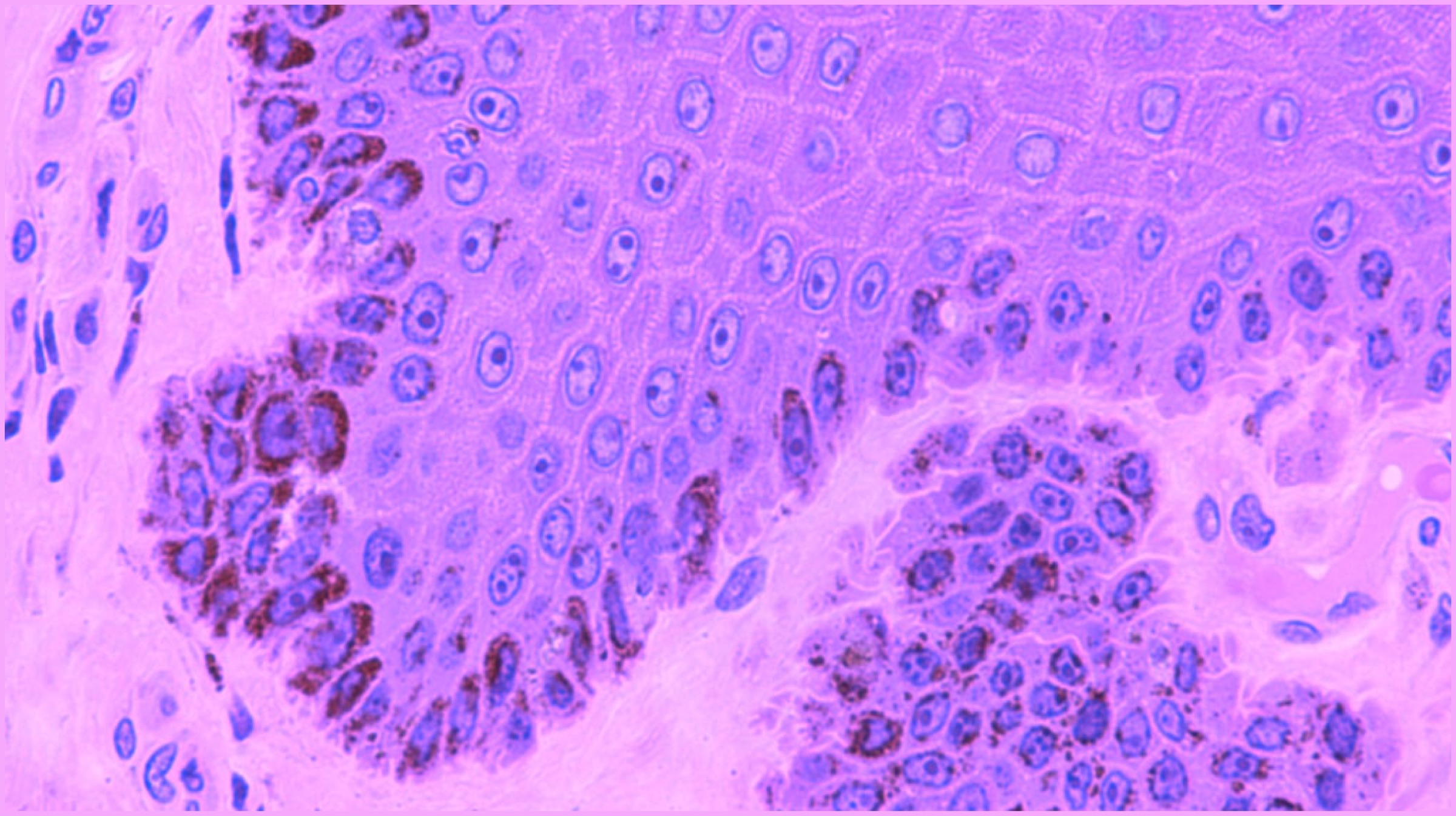 Dr Hornyak and his team of researchers implemented a mouse model to identify a specific version of the melanocyte stem cell. As the name suggests, the cells produce melanin (the pigment that determines the colour of skin and hair) and are present in the hair follicles and skin. These cells have a very unique ability – they can divide limitlessly. In fact, this ability is so unique that it is not present in any other cell in the human body. These stem cells can further develop different types of cells, which depends entirely upon the type of signal provided to them.
Dr Hornyak and his team of researchers implemented a mouse model to identify a specific version of the melanocyte stem cell. As the name suggests, the cells produce melanin (the pigment that determines the colour of skin and hair) and are present in the hair follicles and skin. These cells have a very unique ability – they can divide limitlessly. In fact, this ability is so unique that it is not present in any other cell in the human body. These stem cells can further develop different types of cells, which depends entirely upon the type of signal provided to them. 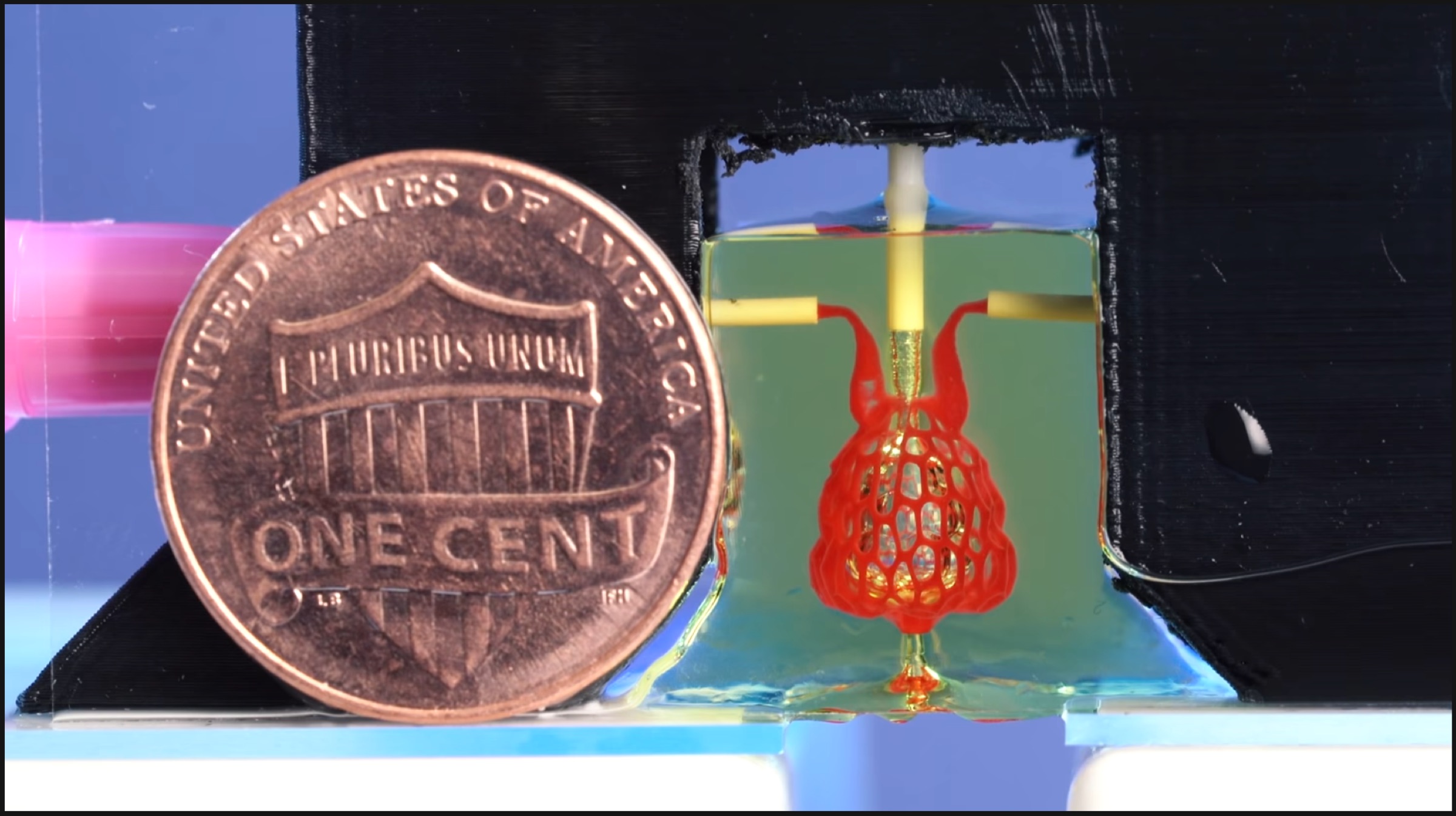
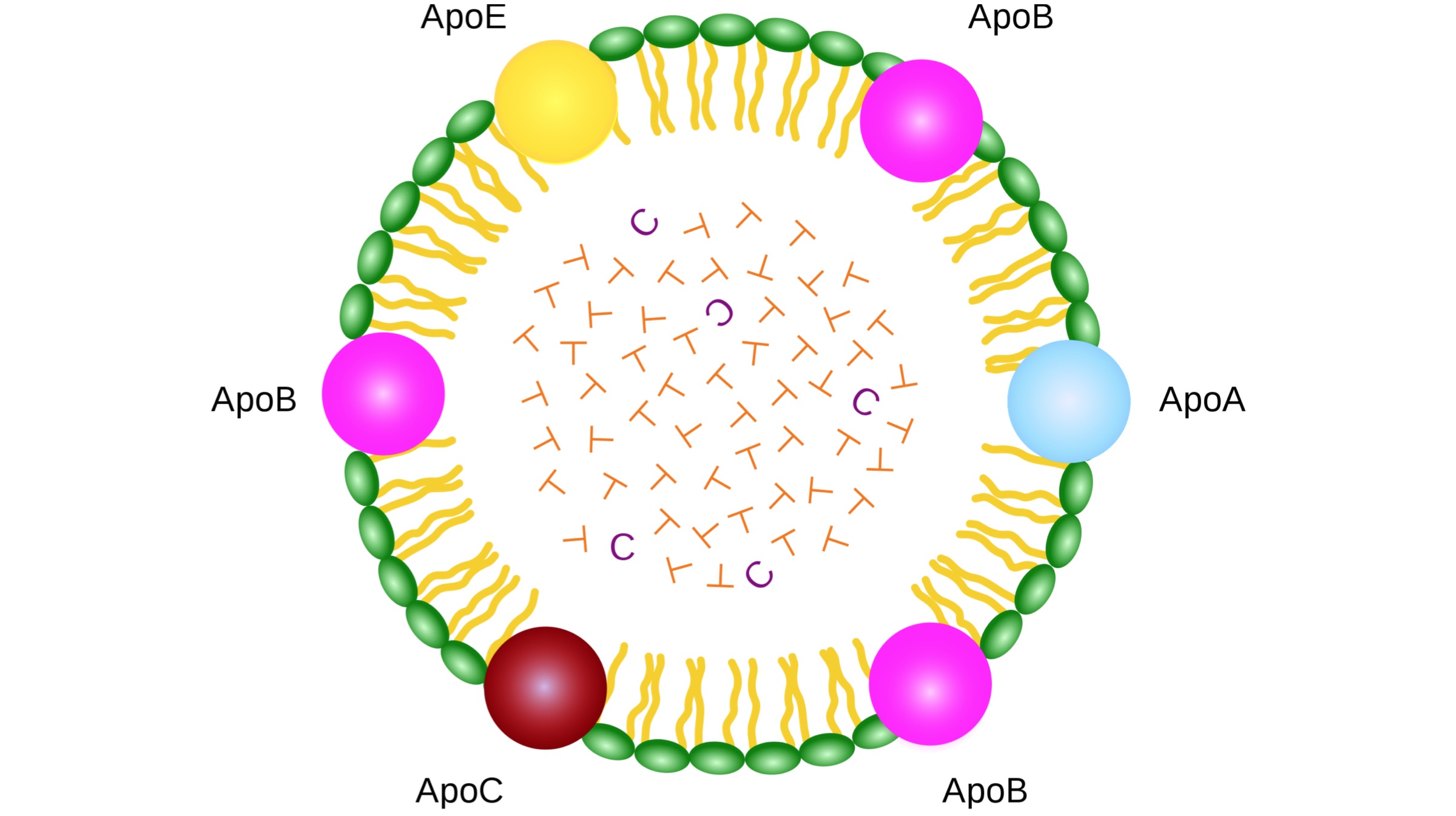
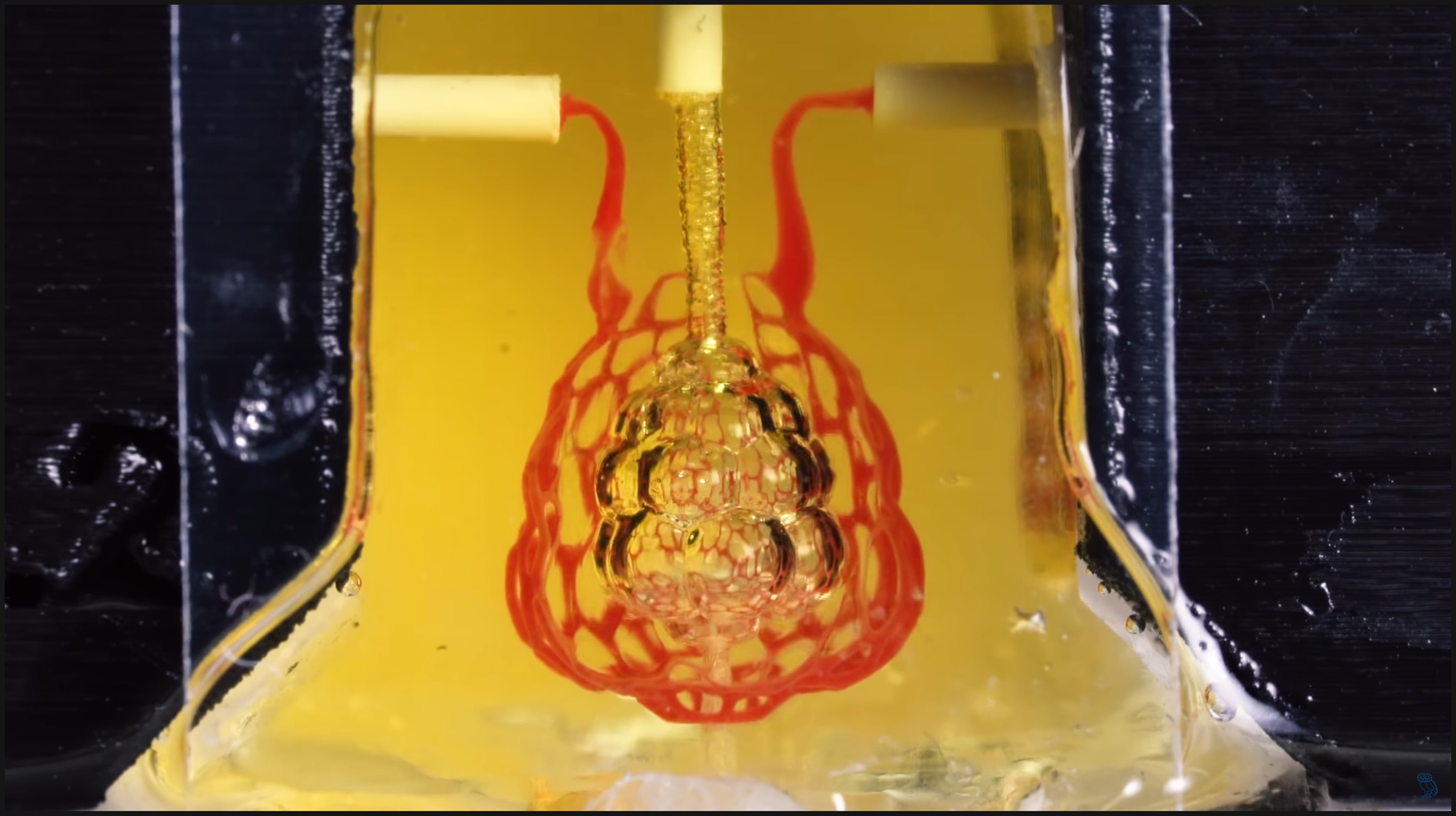 The team was led by bioengineers from Rice University and University of Washington. The 3D printed lung was designed in such a way that it could include independent vascular networks. The different vascular networks include airways, lung blood vessels, bile ducts and the blood vessels present inside the liver. Delivering oxygen to tissues surrounding the blood vessels was always a challenge, but the researchers claim that their bioprinting technology is the first one to beat the hurdle of multivascularization in an artificially designed organ.
The team was led by bioengineers from Rice University and University of Washington. The 3D printed lung was designed in such a way that it could include independent vascular networks. The different vascular networks include airways, lung blood vessels, bile ducts and the blood vessels present inside the liver. Delivering oxygen to tissues surrounding the blood vessels was always a challenge, but the researchers claim that their bioprinting technology is the first one to beat the hurdle of multivascularization in an artificially designed organ. 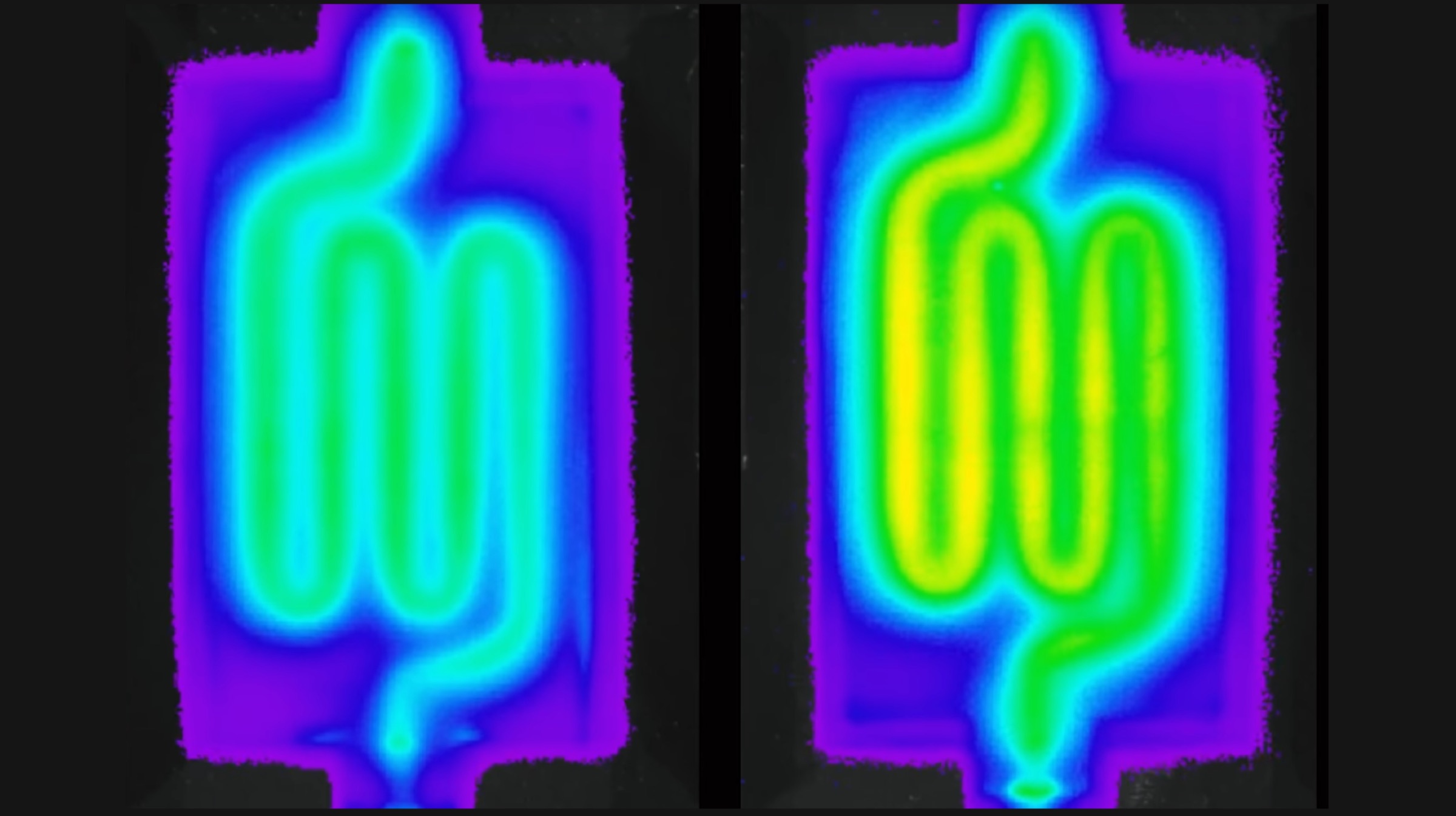 An assistant professor at the University of Washington states that with the removal of such an obstacle from the path, multiple tissues can be designed which can breathe and function just like the healthy tissue in our bodies. Not just that, 3D printed organs will be able to behave more functionally than ever before. Bioprinting has gained a lot of traction in the past few years, solely because it could allow doctors to print replacement organs from a patient’s own cells, increasing chances of survival drastically.
An assistant professor at the University of Washington states that with the removal of such an obstacle from the path, multiple tissues can be designed which can breathe and function just like the healthy tissue in our bodies. Not just that, 3D printed organs will be able to behave more functionally than ever before. Bioprinting has gained a lot of traction in the past few years, solely because it could allow doctors to print replacement organs from a patient’s own cells, increasing chances of survival drastically.  Also Read:
Also Read: 
 Although the disease is not fatal, it’s symptoms may lead to incidents that may be fatal in the long run. As per recent reports, researchers from
Although the disease is not fatal, it’s symptoms may lead to incidents that may be fatal in the long run. As per recent reports, researchers from 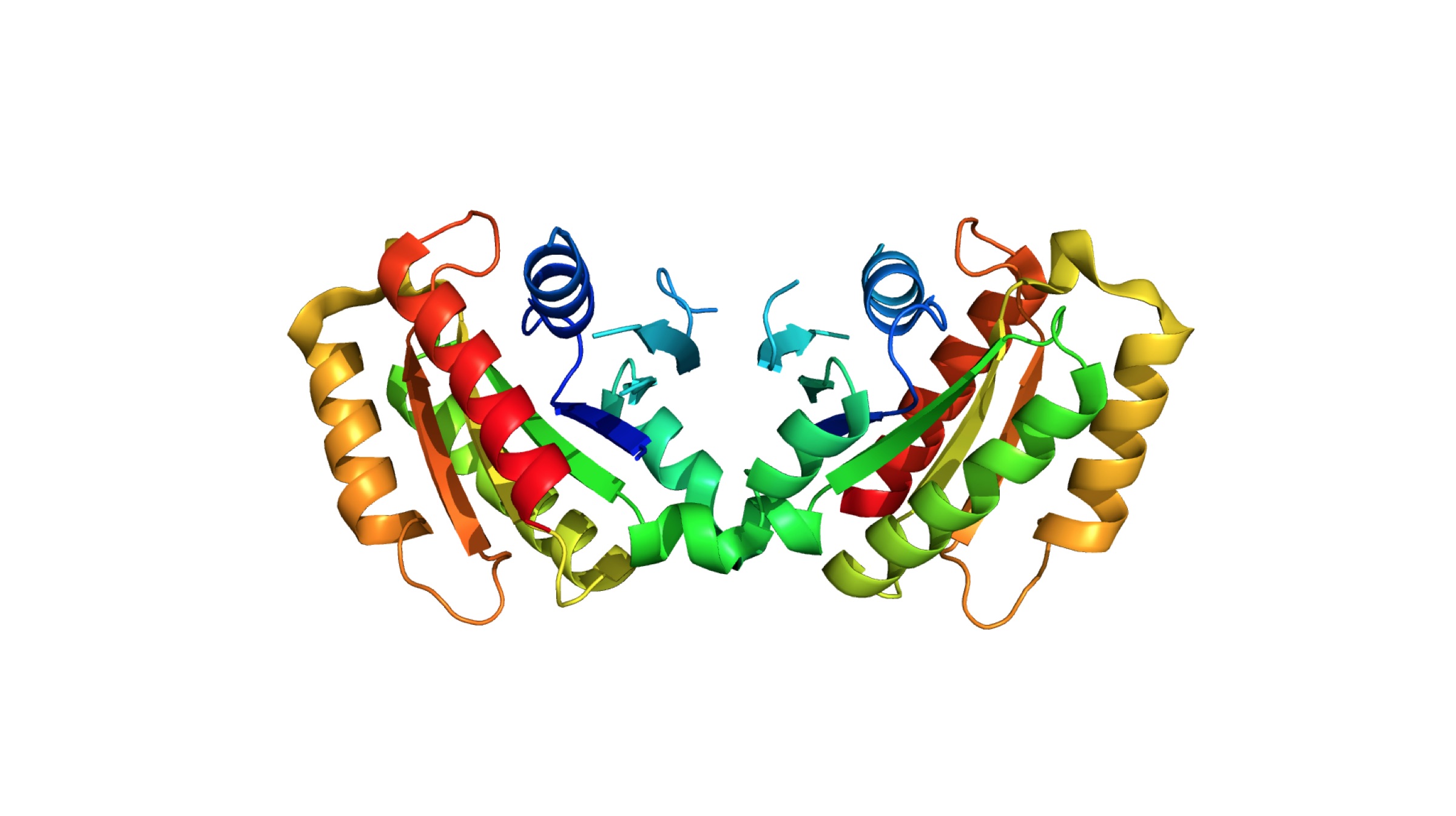 Also Read:
Also Read: 
 The scientists have developed two different types of robotic systems for entirely varied purposes. One of them works on open surfaces, whereas the other system is designed specifically to operate inside closed spaces. The researchers showcased the microrobots’ ability to destroy biofilms and sticky deposits of bacteria. Plus, the scientists state that the same technology can be implemented in cleaning dirty water pipes and other inaccessible areas which are prone to bacterial deposits.
The scientists have developed two different types of robotic systems for entirely varied purposes. One of them works on open surfaces, whereas the other system is designed specifically to operate inside closed spaces. The researchers showcased the microrobots’ ability to destroy biofilms and sticky deposits of bacteria. Plus, the scientists state that the same technology can be implemented in cleaning dirty water pipes and other inaccessible areas which are prone to bacterial deposits.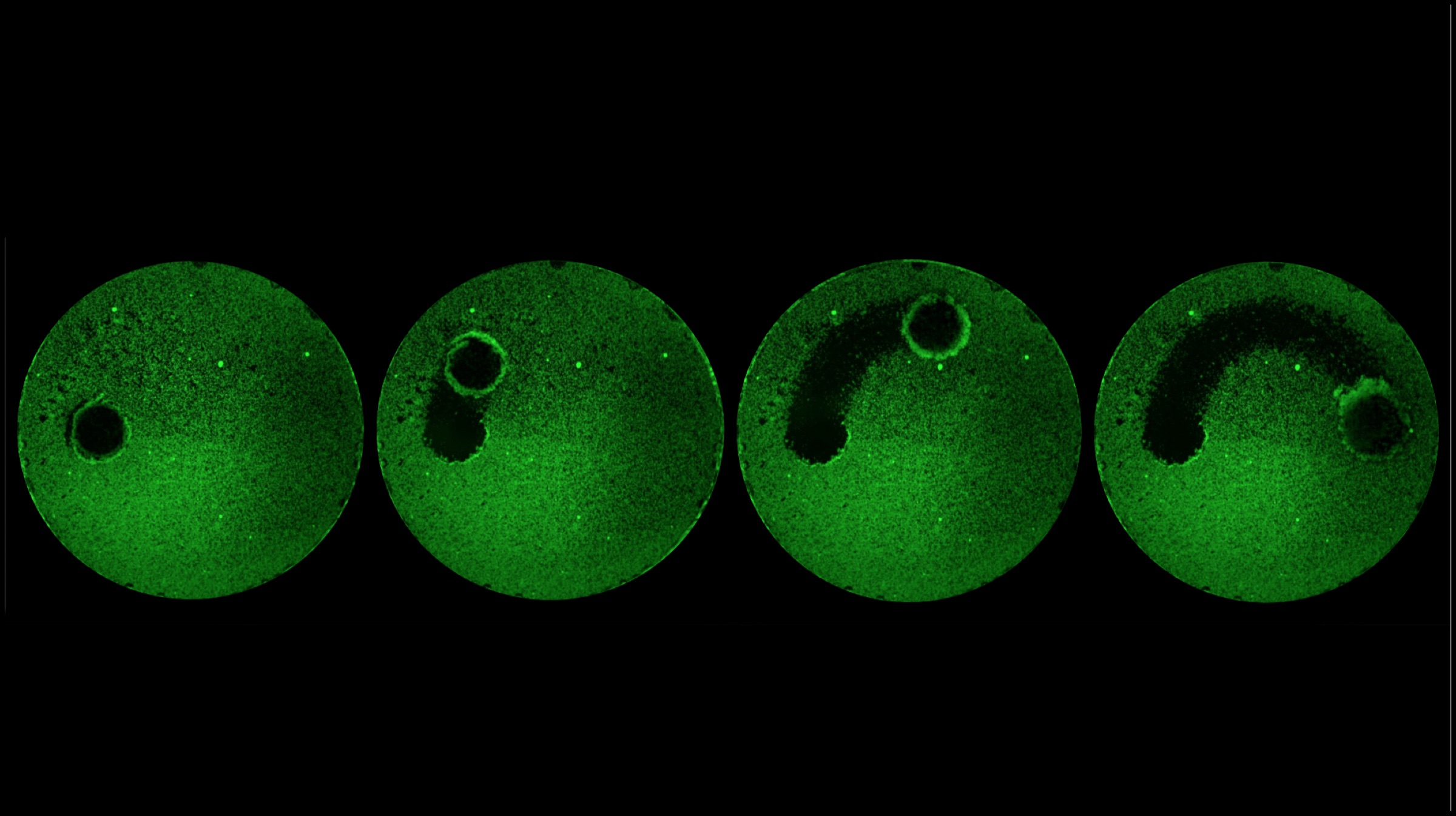 Also Read:
Also Read: 
 The design of the 3D printed microscope is based on digital holographic microscopy. Bahram claims that the images produced by the portable microscope are almost twice the resolution of the images produced by traditional microscopy. The applications of such a device are not limited to research and medical science, rather, it can be used in defence and education as well. Since the entire microscope is manufactured out of 3D printed parts, it can be assembled anywhere and with relative ease. Moreover, unlike other scientific equipment, the 3D printed microscope is not expensive at all. Also, the incorporation of alternative components such as image sensors could drastically reduce the price point of the microscope when/if it is mass produced at some point.
The design of the 3D printed microscope is based on digital holographic microscopy. Bahram claims that the images produced by the portable microscope are almost twice the resolution of the images produced by traditional microscopy. The applications of such a device are not limited to research and medical science, rather, it can be used in defence and education as well. Since the entire microscope is manufactured out of 3D printed parts, it can be assembled anywhere and with relative ease. Moreover, unlike other scientific equipment, the 3D printed microscope is not expensive at all. Also, the incorporation of alternative components such as image sensors could drastically reduce the price point of the microscope when/if it is mass produced at some point.  The core of the new microscope works in similar ways to a traditional digital holographic ones, where a digital camera captures the hologram generated when the light coming from the sample object interferes or colludes with the reference light wave. This process relies on a controlled setup where the environment has to be free of vibrations and temperature fluctuations. Instead, the newly manufactured equipment combines the two images using a super-resolution technique, which is scientifically referred to as Structured Illumination Microscopy. In this process, a structured light pattern is created with the help of a clear disc.
The core of the new microscope works in similar ways to a traditional digital holographic ones, where a digital camera captures the hologram generated when the light coming from the sample object interferes or colludes with the reference light wave. This process relies on a controlled setup where the environment has to be free of vibrations and temperature fluctuations. Instead, the newly manufactured equipment combines the two images using a super-resolution technique, which is scientifically referred to as Structured Illumination Microscopy. In this process, a structured light pattern is created with the help of a clear disc.  Also Read:
Also Read: 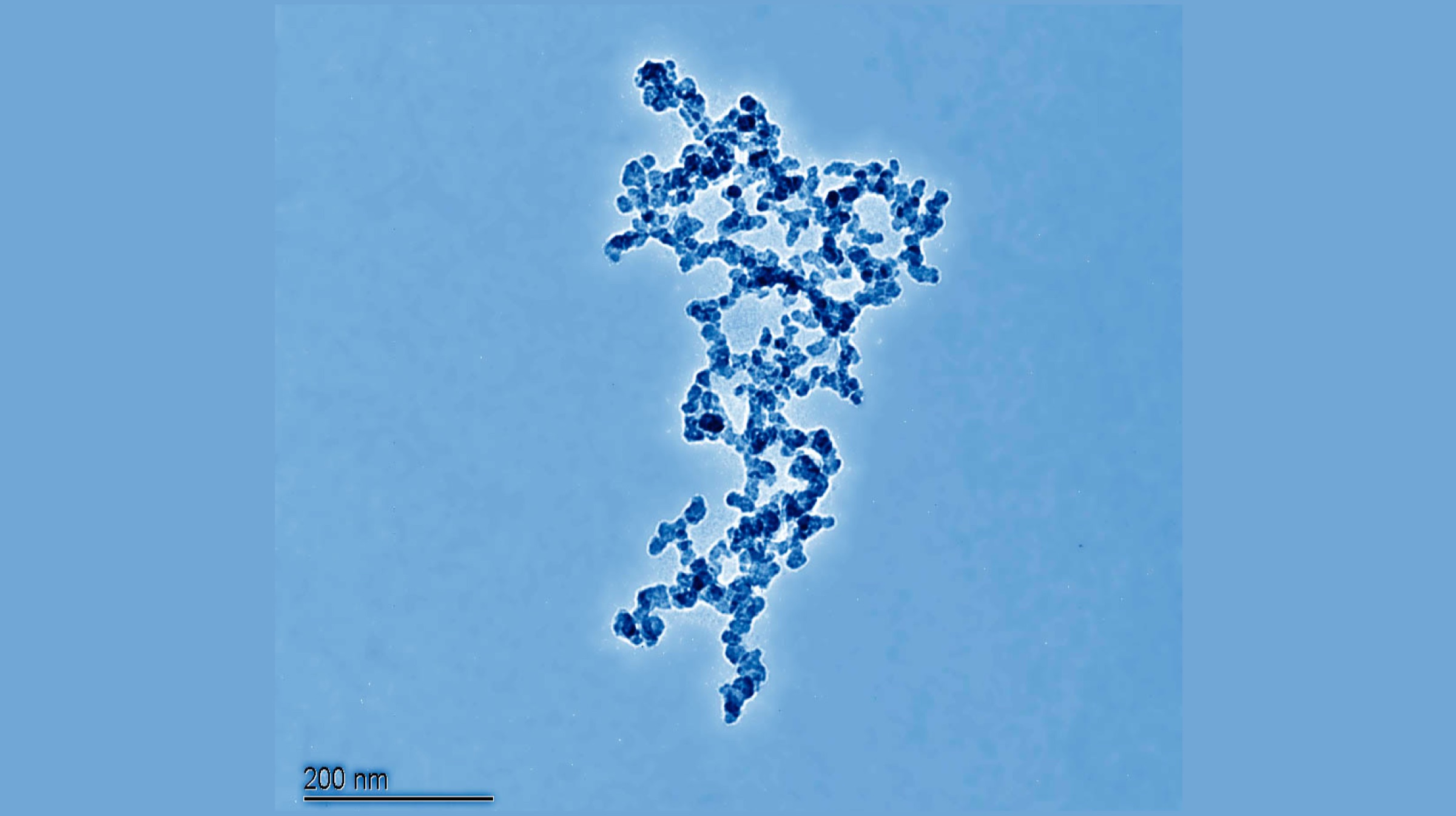
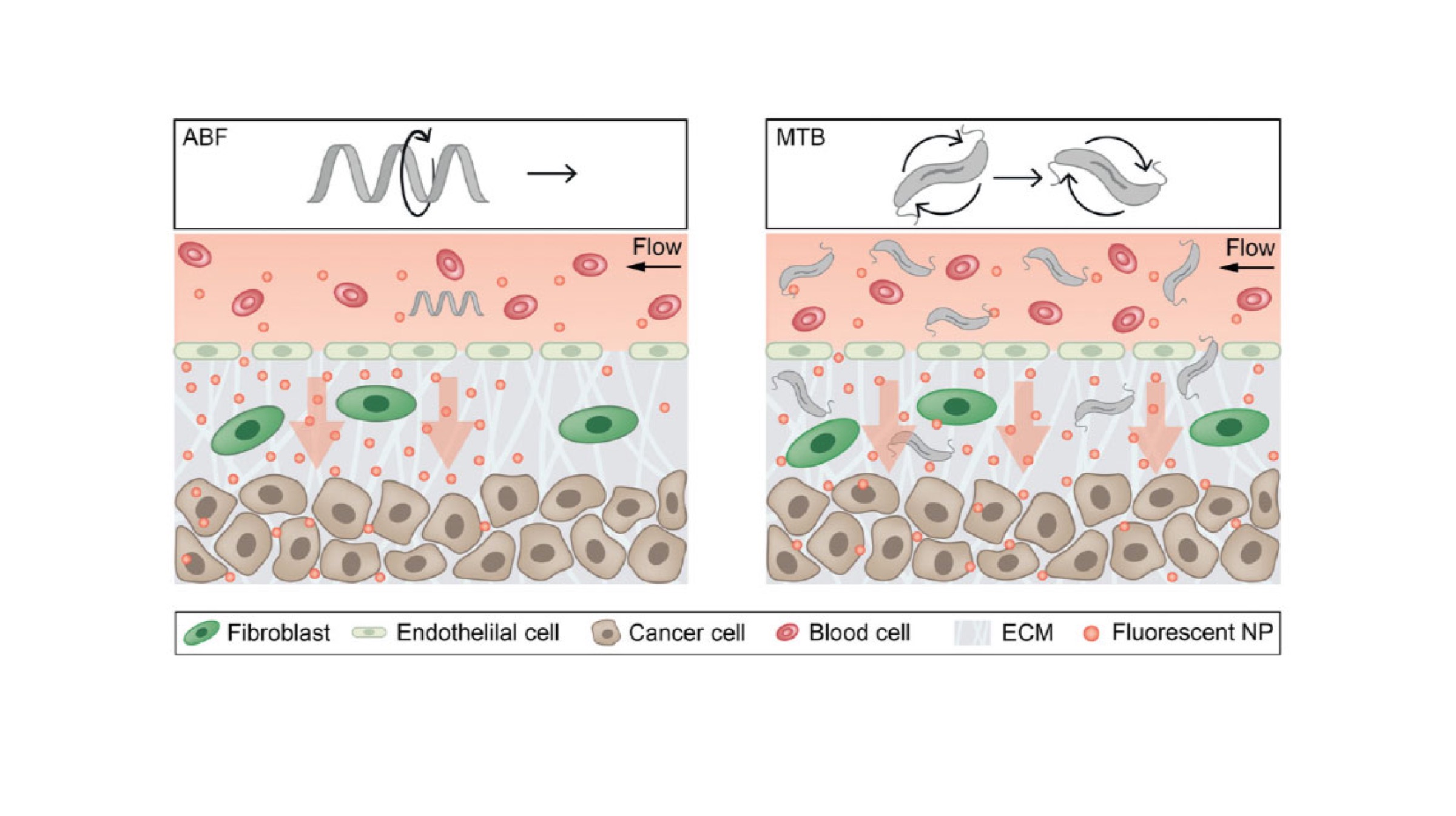 One of the biggest challenges while delivering drugs via nanoparticles is the exit strategy of the robots, implying that the micro robots can escape the blood vessels and accumulate in the desired spot for removal from the human body. Sangeeta Bhatia, a senior author of the aforementioned study states that it is tough to get the nanomaterials to the tissue in the lining of the blood vessel, but the use of magnetism to develop fluid forces, the nanoparticles can be pushed through the lining. The same study further states that swarms of naturally magnetic bacteria (Magnetotactic bacteria) can be also used to achieve the same result.
One of the biggest challenges while delivering drugs via nanoparticles is the exit strategy of the robots, implying that the micro robots can escape the blood vessels and accumulate in the desired spot for removal from the human body. Sangeeta Bhatia, a senior author of the aforementioned study states that it is tough to get the nanomaterials to the tissue in the lining of the blood vessel, but the use of magnetism to develop fluid forces, the nanoparticles can be pushed through the lining. The same study further states that swarms of naturally magnetic bacteria (Magnetotactic bacteria) can be also used to achieve the same result. Schurele, the assistant professor at the Swiss Federal Institute of Technology previously worked on magnetic microbots, and consequently she aimed towards making the nanoparticle drug delivery technique more efficient when she started working with Sangeeta Bhatia. The researchers used their micro robots to target diseased sites in the human body which were usually a host of tumours. Since they faced issues with the same, the team explored their options with magnetic bacteria to devise a method to push the particles to the target in a better way.
Schurele, the assistant professor at the Swiss Federal Institute of Technology previously worked on magnetic microbots, and consequently she aimed towards making the nanoparticle drug delivery technique more efficient when she started working with Sangeeta Bhatia. The researchers used their micro robots to target diseased sites in the human body which were usually a host of tumours. Since they faced issues with the same, the team explored their options with magnetic bacteria to devise a method to push the particles to the target in a better way.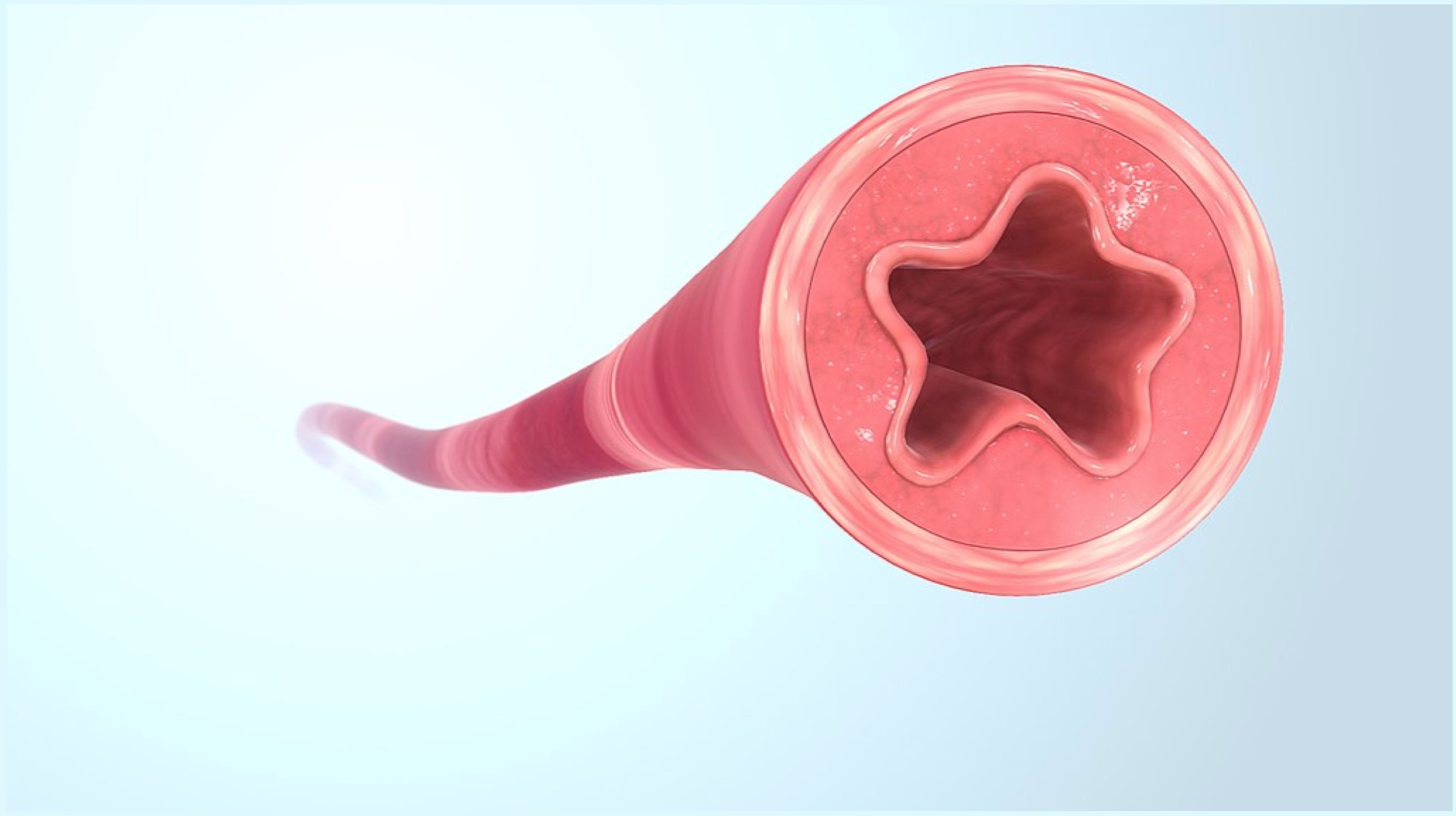 Also Read:
Also Read: 
 Dr. Niklas Mattsson, the physician at Skåne University Hospital and the lead author of the aforementioned study stated that a protein called neurofilament light in the blood can be conveniently used to measure brain cell damage in various stages of Alzheimer’s disease. The protein leaks/spills out of damaged and dying nerve cells and travels into the cerebrospinal fluid, heading into the bloodstream shortly afterwards. As per previous studies, people who suffer from diseases like Alzheimer’s have a higher level of neurofilament light in the blood.
Dr. Niklas Mattsson, the physician at Skåne University Hospital and the lead author of the aforementioned study stated that a protein called neurofilament light in the blood can be conveniently used to measure brain cell damage in various stages of Alzheimer’s disease. The protein leaks/spills out of damaged and dying nerve cells and travels into the cerebrospinal fluid, heading into the bloodstream shortly afterwards. As per previous studies, people who suffer from diseases like Alzheimer’s have a higher level of neurofilament light in the blood. Also Read:
Also Read: 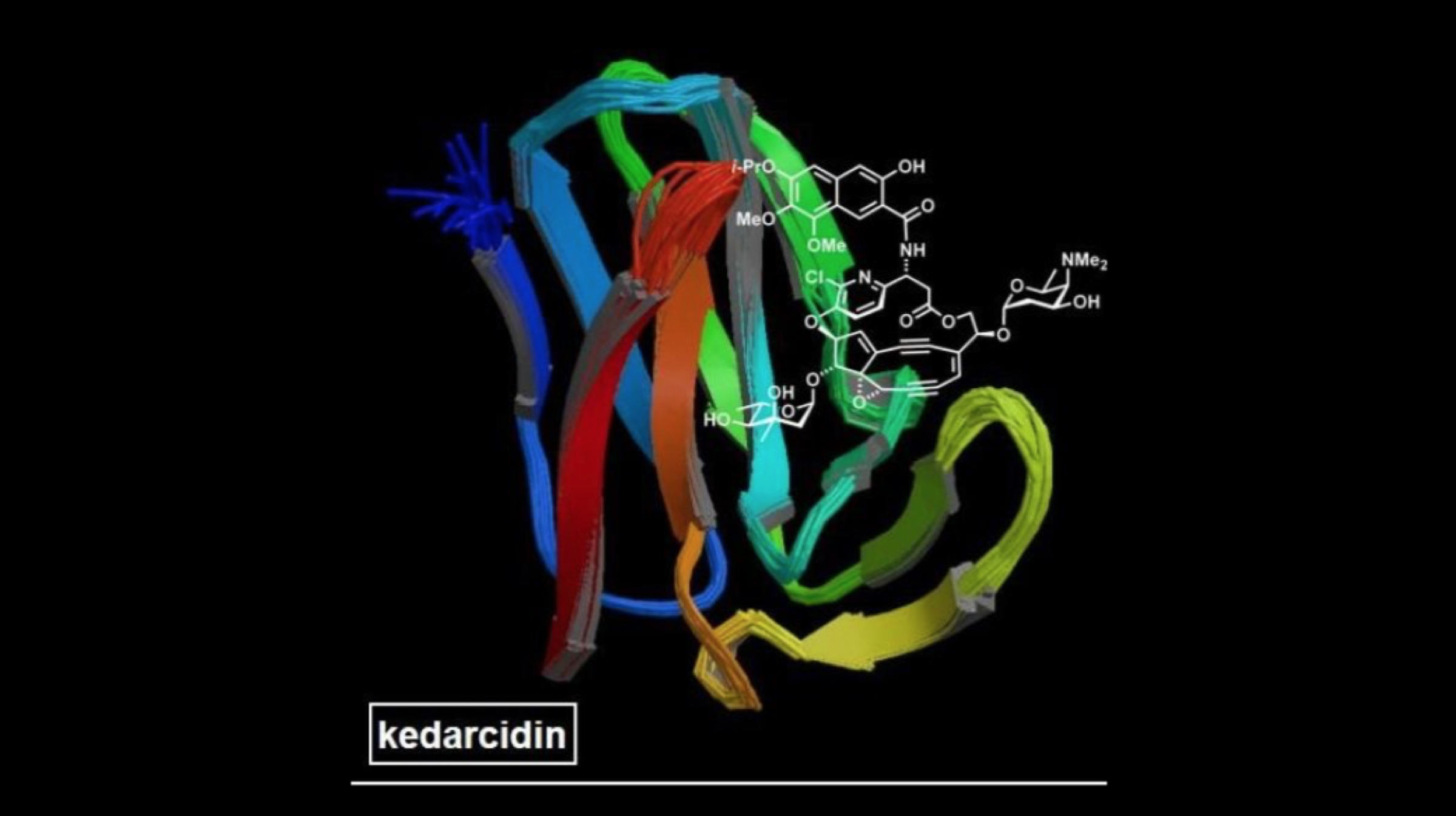
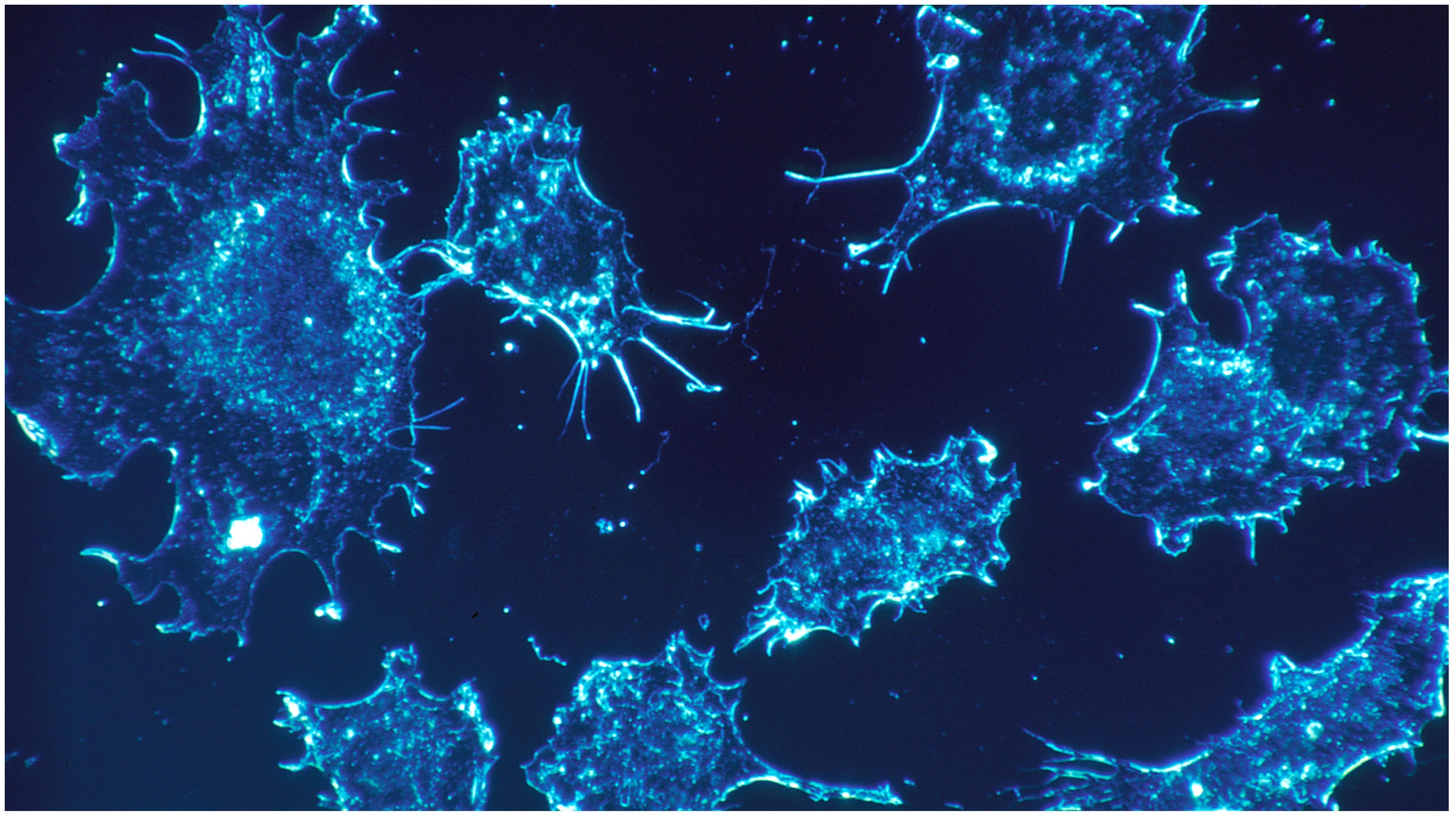
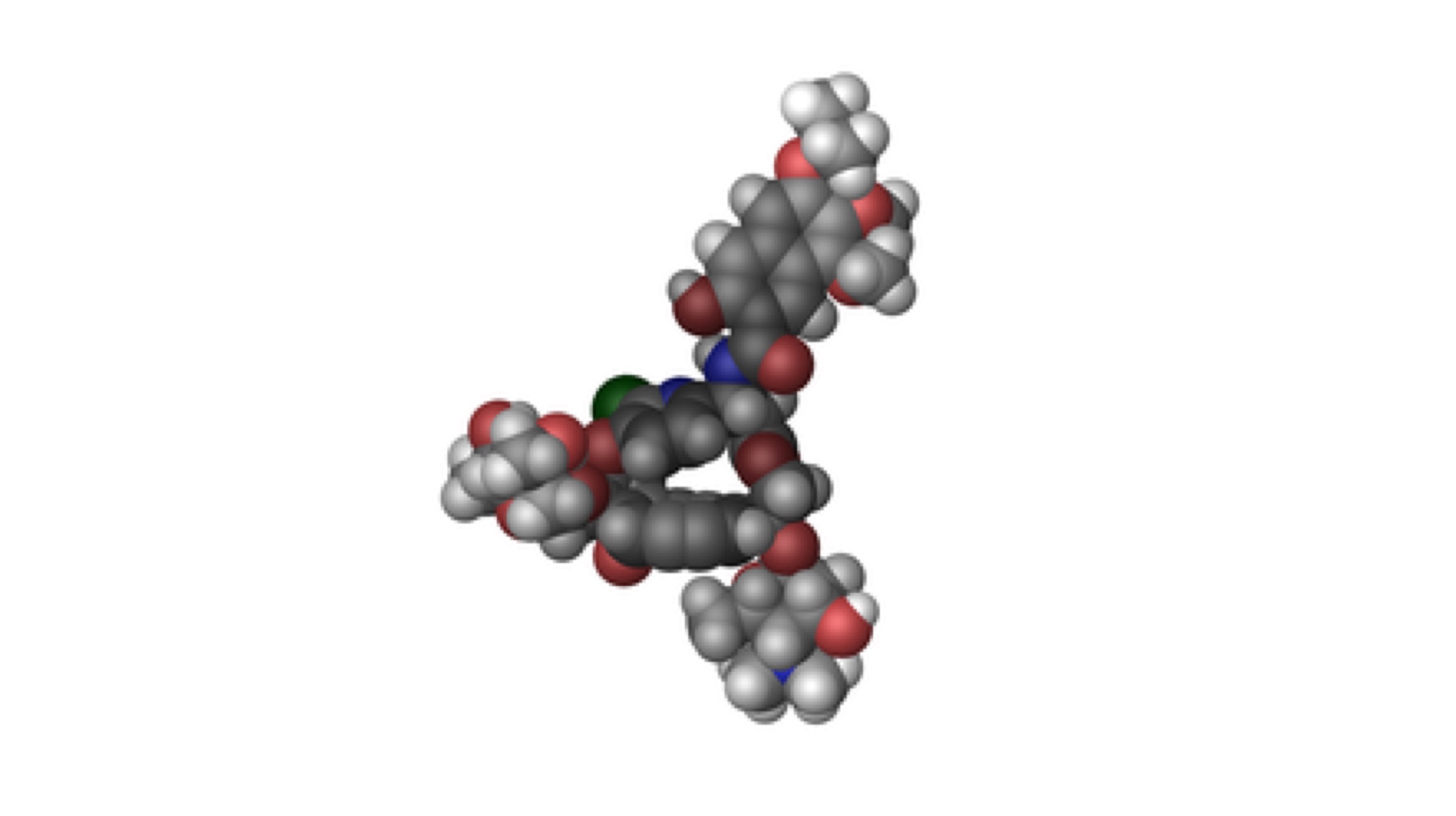 The antibiotic, or rather, the “super-substance” is called Kedarcidin. It was first discovered almost 30 years ago by a pharmaceutical company in India. Extracted from a soil sample, Kedarcidin’s natural form was unusable as a potential drug to fight cancer. In fact, most antibiotics developed in the last 70 years have been derived out of soil, but in order to use them as a drug for treatments, the antibiotics have to be reproduced via the process of chemical synthesis in the laboratory. Kedarcidin, however, is different from conventional antibiotics.
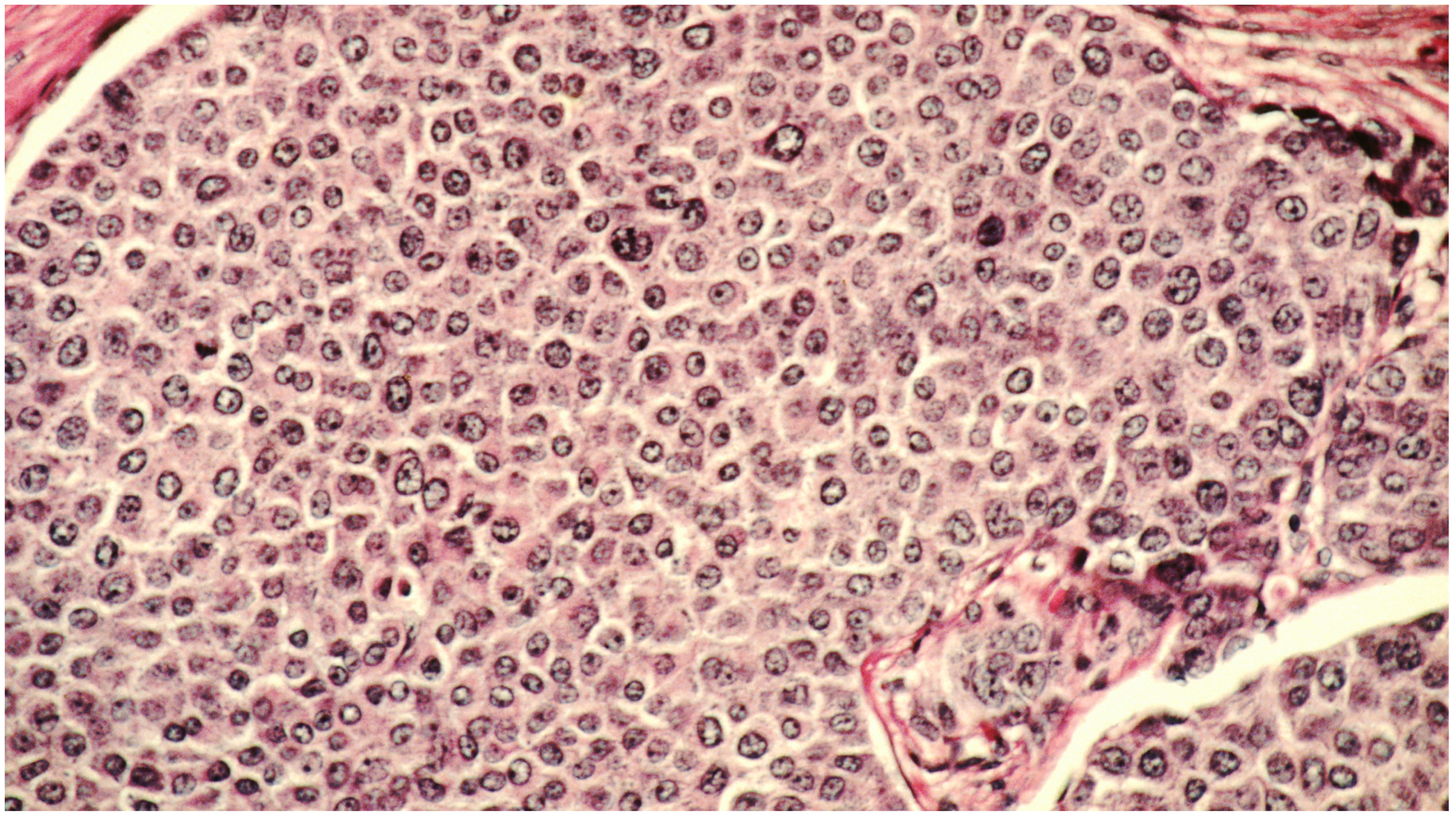
The antibiotic, or rather, the “super-substance” is called Kedarcidin. It was first discovered almost 30 years ago by a pharmaceutical company in India. Extracted from a soil sample, Kedarcidin’s natural form was unusable as a potential drug to fight cancer. In fact, most antibiotics developed in the last 70 years have been derived out of soil, but in order to use them as a drug for treatments, the antibiotics have to be reproduced via the process of chemical synthesis in the laboratory. Kedarcidin, however, is different from conventional antibiotics.  For starters, Kedarcidin is capable of harming tumour cells instead of just killing the bacteria involved (like many other antibiotics). This makes it a very potential candidate as a primary drug in effective cancer treatments. The biological structure of Kedarcidin enables it to harm the DNA structure of the target tumour to a level of complexity that the tumour cannot spread at all. Because of the complex structure of Kedarcidin, scientists were unable to replicate it’s “potential drug” form, until now.
For starters, Kedarcidin is capable of harming tumour cells instead of just killing the bacteria involved (like many other antibiotics). This makes it a very potential candidate as a primary drug in effective cancer treatments. The biological structure of Kedarcidin enables it to harm the DNA structure of the target tumour to a level of complexity that the tumour cannot spread at all. Because of the complex structure of Kedarcidin, scientists were unable to replicate it’s “potential drug” form, until now.